ABG interpretation
Notes
Overview
Interpretation of an arterial blood gas is an essential skill required by all doctors and most healthcare professionals.
In simplistic terms, an arterial blood gas (ABG) tells us about three main things:
- Oxygenation: measurement of oxygen within the blood.
- Ventilation: process of respiratory function (i.e. breathing).
- Acid-base balance: the control of pH.
To enable us to interpret oxygenation, respiratory function and acid-base balance, an ABG analyser gives us key bits of information. This includes the pH, partial pressure of oxygen, partial pressure of carbon dioxide and calculated bicarbonate.
Key components
- pH (normal range 7.35-7.45): refers to the acidity or alkalinity of the blood. Tight control needed for normal metabolic function.
- PaCO2 (normal range 4.7-6.0 kPa / 35–45 mmHg): partial pressure of arterial carbon dioxide. Essentially the concentration of carbon dioxide in the blood. Altered by respiration and therefore provides the ‘respiratory’ component of the blood gas.
- PaO2 (normal range 10.6–13.3 kPa / 80–100 mmHg): partial pressure of arterial oxygen. Essentially the concentration of oxygen in the blood.
- HCO3- (normal range 22-26 mmol/L): calculated bicarbonate level. Bicarbonate is an important buffer of acids. Regulated by the kidneys. Therefore, provides the ‘metabolic’ component of the blood gas.
- Base excess (normal range +2 to -2 mmol/L): measures ‘excess’ amount or ‘deficit’ amount of an acid or base. The term negative base excess often used instead of base deficit.
Using these parameters, an ABG can give us information about what is going on inside the body and the likely cause of dysfunction.
Additional components
In modern medicine, an ABG can give us a wealth of additional information, including:
- Electrolytes: sodium (Na+), potassium (K+), chloride (Cl-), ionised calcium (Ca2+)
- Creatinine (some analysers)
- Lactate: byproduct of anaerobic respiration that is useful as a marker of tissue perfusion
- Haemoglobin and derivatives (e.g. carboxyhemoglobin, methaemoglobin)
- Blood glucose level
Control of pH
Within the body, pH is tightly regulated by chemical buffers, the respiratory system and renal system.
Understanding how the body tightly controls pH through the respiratory and renal systems is important for ABG interpretation.
For more information, see our notes on pH control.
As a brief summary:
- Respiratory system (quick response): controls pH through altered of carbon dioxide. Increasing ventilation lower carbon dioxide level and therefore increases pH. Decreasing ventilation raises carbon dioxide level and therefore decreases pH.
- Renal system (delayed response): controls pH through secretion of hydrogen ions and reabsorption of bicarbonate. If both increased, pH rises. If both decreased, pH falls.
Stepwise approach
When interpreting an ABG, it is important to use the same stepwise approach.
- Determine oxygenation (PaO2)
- Determine pH (acidosis or alkalosis)
- Determine respiratory component (PaCO2)
- Determine metabolic component (Bicarbonate)
- Determine compensation
- Final interpretation
- Review other parameters
Step 1: Oxygenation
The normal partial pressure of oxygen (PaO2) is approximately 10.6–13.3 kPa.
Step 1 involves checking whether the patient has hypoxaemia (low blood oxygen levels).
Firstly, check if the patient is receiving supplemental oxygen. This is represented as a percentage (e.g. 24%, 60%). Room air is represented as 21%, which is the partial pressure of oxygen at atmospheric pressure.
The PaO2 is always lower than alveoli oxygen. Therefore, it is estimated that the Pa02 should be 10 less than the inspired oxygen (e.g. 11 kPa breathing at 21% room air).
Examples
- If inspired oxygen is 35% via venturi mask, PaO2 should be roughly 25 kPa
- If inspired oxygen at 60% via humidified oxygen, PaO2 should be roughly 50 kPa
- If inspired oxygen at 24% nasal cannula, PaO2 should be roughly 14 kPa
Key values
- Hypoxaemia: PaO2 < 10.6 kPa or difference between inspired oxygen and PaO2 > 10
- Type 1 respiratory failure: PaO2 < 8 kPa
- Type 2 respiratory failure: PaO2 < 8 kPa in association with raised PaCO2
Step 2: Acid-base balance (pH)
The normal arterial pH is 7.35-7.45.
Step 2 involves checking whether the patient is ‘acidotic’ or ‘alkalotic’
- Acidosis: pH <7.35
- Alkalosis: pH >7.45
Step 3: Respiratory component
The respiratory component of the ABG refers to the partial pressure of carbon dioxide (normal range 4.7-6.0 kPa).
Step 3 involves checking the PaCO2, which is a reflection of the respiratory contribution to acid-base regulation or ‘pH control’. The PaCO2 needs to be check in context of the pH.
- Acidosis (pH <7.35) and raised PaCO2 (> 6.0 kPa): suggest primary respiratory acidosis (high CO2 contributing to acid load). If bicarbonate is also low, suggest mixed respiratory and metabolic acidosis.
- Alkalosis (pH >7.45) and low PaCO2 (< 4.7 kPa): suggests primary respiratory alkalosis (low CO2 causes a lower acid load). If bicarbonate also high, reflects respiratory and metabolic alkalosis.
Step 4: Metabolic component
The metabolic component of the ABG refers to the bicarbonate level (normal range 22-26 mmol/L).
Step 4 involves checking the bicarbonate level, which is a reflection of the renal (or ‘metabolic) contribution to pH control. Needs to be assessed in context of the pH and PaCO2.
- Acidosis (pH < 7.35) and bicarbonate decreased (< 22 mmol/L): suggests primary metabolic acidosis (bicarbonate falls trying to buffer excess hydrogen ions). If the PaCO2 is also raised, would be a mixed respiratory and metabolic acidosis.
- Alkalosis (pH >7.45) and bicarbonate increased (>26 mmol/L): suggests primary metabolic alkalosis. If the PaCO2 is also low, would be a mixed respiratory and metabolic alkalosis.
Base excess/deficit is often used interchangeably with bicarbonate as a marker of the metabolic contribution to pH control.
- Base deficit (< -2 mmol/L): used as a marker of low bicarbonate level
- Base excess (> +2 mmol/L): used as a marker of high bicarbonate level
Step 5: Compensation
Compensation refers to the appropriate attempt of the respiratory or renal systems to restore pH.
Both respiratory compensation and metabolic compensation can occur depending on the acid-base abnormality. Respiratory compensation, through alteration of carbon dioxide, is a quick mechanism. Metabolic (i.e. renal) compensation through alteration of bicarbonate is a delayed mechanism.
Respiratory compensation
- Acidosis (pH <7.35) and low PaCO2 (< 4.7 kPa): suggests respiratory compensation to acidosis (trying to compensate by reducing CO2 and thus acid load). Seen in metabolic acidosis.
- Alkalosis (pH >7.45) and high PaCO2 (> 6.0 kPa): suggests respiratory compensation to alkalosis (trying to compensate by increasing CO2 and thus acid load). Seen in metabolic alkalosis.
Metabolic compensation
- Acidosis (pH < 7.35) and bicarbonate increased (>26 mmol/L): suggests metabolic compensation to acidosis (trying to conserve bicarbonate ions to buffer hydrogen ions). Seen in respiratory acidosis.
- Alkalosis (pH >7.45) and bicarbonate decreased (< 22 mmol/L): suggests metabolic compensation to alkalosis (trying to reduce bicarbonate levels to prevent hydrogen ion buffering). Seen in respiratory alkalosis.
Step 6: Final interpretation
Final interpretation should state the contribution of respiratory and metabolic systems and presence of compensation.
Respiratory or metabolic component
- Metabolic acidosis
- Metabolic alkalosis
- Respiratory acidosis
- Respiratory alkalosis
- Mixed (e.g. metabolic and respiratory acidosis)
With mixed results, it is useful to determine which is the predominant abnormality (respiratory or metabolic).
Compensation
- Not compensated: no evidence of appropriate respiratory or metabolic compensation. For example, no rise in bicarbonate in respiratory acidosis.
- Partial compensation: evidence of appropriate respiratory or metabolic compensation, but pH not restored to normal. For example, a fall in PaCO2 in context of metabolic acidosis (pH 7.30, PaCO2 3.5, HCO3- 15).
- Complete compensation: evidence of appropriate respiratory or metabolic compensation and restoration of normal pH. For example, chronic respiratory acidosis with significantly elevated bicarbonate level (pH 7.36, PaCO2 8.3, HCO3- 38).
Interpretation example
Mrs Smith’s arterial blood gas on 35% inspired oxygen
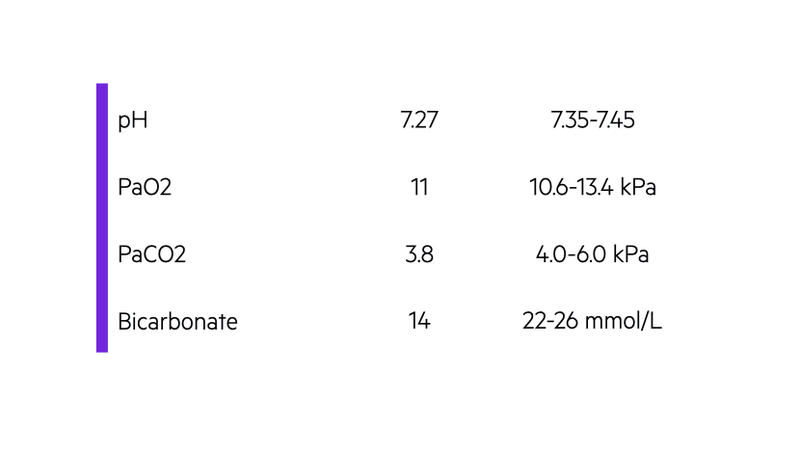
Mrs Smith has hypoxaemia (inappropriately low PaO2 for inspired oxygen) with a metabolic acidosis (low pH, low bicarbonate) and evidence of partial respiratory compensation (low PaCO2 in response to acidosis).
Step 7: Review other parameters
Modern blood gas analysers give a wealth of additional information.
Make sure you look at the additional information provided to you on a blood gas analysis. There could be multiple abnormalities including electrolyte disturbances, acute kidney injury, raised blood glucose or significant anaemia.
Last updated: November 2021
Have comments about these notes? Leave us feedback
