Respiratory alkalosis
Notes
Overview
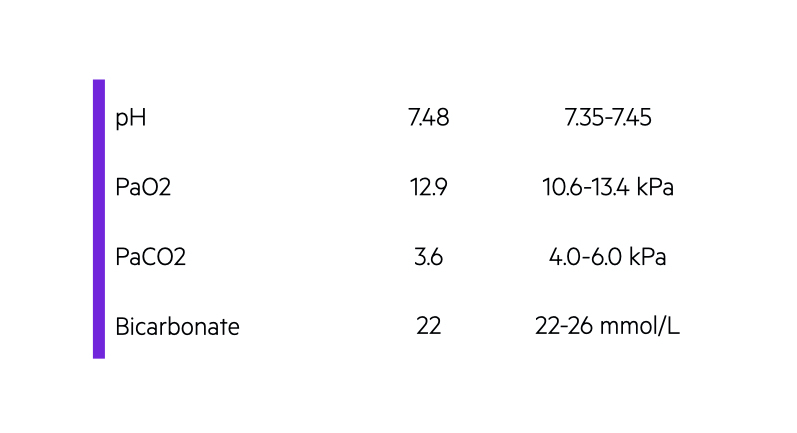
Respiratory alkalosis is characterised by a pH > 7.45 and low partial pressure of arterial carbon dioxide (< 4 kPa).
Respiratory alkalosis primarily occurs as a result of increased clearance of carbon dioxide from the lungs. It is commonly seen as a compensatory response to metabolic acidosis. Alternatively, it can occur as a primary abnormality (e.g. pulmonary embolism). It is characterised by alkalosis (pH > 7.45) and a low PaCO2 (< 4 kPa).
The principle mechanism of respiratory alkalosis, regardless of whether it is compensatory or primary, is hyperventilation. This refers to an increase in alveolar ventilation, which leads to clearance or ‘blowing off’ of carbon dioxide. It is the most common acid-base abnormality in patients who are critically unwell.
Chemoreceptors
Central and peripheral chemoreceptors detect changes in hydrogen ion concentration and thus pH.
The concentration of carbon dioxide in the blood is tightly controlled and regulated by chemoreceptors within brain (central) and carotid bodies (peripheral).
Fluctuations in hydrogen ion concentration is sensed by chemoreceptors and ventilation altered to adjust the level of PaCO2. If hydrogen ions increase, chemoreceptors stimulate an increase in ventilation. This subsequently ’blows off’ more carbon dioxide and normal pH is restored
Aetiology
Several underlying causes can stimulate an increase in ventilation leading to a fall in PaCO2 and respiratory alkalosis.
The broad causes of respiratory alkalosis include:
- Increased stimulation of respiratory drive: cerebral disease (e.g. head injury, mass, stroke), systemic illness (e.g. sepsis, hyperthermia), medications.
- Hypoxaemia-induced (low PaO2): detected by peripheral chemoreceptors, drive hyperventilation. Classically due to pulmonary disease (e.g. asthma, pneumonia, pulmonary embolism) and cardiac disease (e.g. congenital heart disease, shock)
- Iatrogenic (accidental or intentional): due to alteration in ventilation settings in patients mechanically ventilated.
- Hyperventilation syndrome: typical presentation of hyperventilation in association with acute anxiety or panic attack. May be an underlying psychiatric history.
Due to the wide variety of possible causes, it is important to fully assess a patient with respiratory alkalosis. This will help to determine what is most likely driving the hyperventilation. Further investigations are guided by the suspected aetiology.
Carbon dioxide and ICP
Respiratory alkalosis may be induced to reduce intracranial pressure (ICP).
Hypercapnia causes cerebral arterial vasodilatation, which increases cerebral blood flow. This results in increased intracranial pressure (ICP). Therefore, in patients who are mechanically ventilated ICP can be reduced by increasing ventilation and subsequently reducing PaCO2. This induces respiratory alkalosis and promotes arterial vasoconstriction.
In patients presenting with acute respiratory alkalosis, and thus hypocapnia, the effect on cerebral blood flow may cause a variety of neurological symptoms. Acute hypocapnia causes cerebral vasoconstriction and reduced cerebral blood flow. This can cause dizziness, altered mental status, syncope and even seizures.
Hyperventilation & electrolytes
Hyperventilation and subsequent respiratory alkalosis can have a profound effect on serum electrolytes.
Hyperventilation is defined as increased ventilation (i.e. over-breathing) in excess of the metabolic needs of the body (i.e. in excess of carbon dioxide production). This leads to removal of carbon dioxide (hypocapnia) and subsequent respiratory alkalosis. This causes a number of somatic symptoms due to alteration in serum electrolytes. In particular, prolonged respiratory alkalosis can lead to secondary hypocalcaemia, hypokalaemia and hypophosphataemia.
Hypocalcaemia and hypokalaemia can lead to a variety of clinical manifestations including cardiac arrhythmias, conduction abnormalities, and various somatic symptoms (e.g. paraesthesia, hyperreflexia, muscle spasm). The higher pH enhances calcium binding to proteins like albumin leading to a fall in serum concentration. Patients often have classical symptoms of perioral and finger paraesthesia. Falls in potassium and phosphate ions occur due to intracellular shifts.
Last updated: March 2021
Have comments about these notes? Leave us feedback
