Trichomoniasis
Notes
Overview
Trichomoniasis is a sexually transmitted infection caused by the protozoan Trichomonas vaginalis.
Trichomoniasis is a sexually transmitted infection (STI), which can affect both men and women. It classically causes vaginal discharge in women and urethral discharge in men, which is associated with soreness (due to vulvovaginitis or urethritis) and/or dysuria.
Epidemiology
Trichomoniasis is the most common non-viral sexually transmitted infections worldwide.
Worldwide, trichomoniasis is extremely common but in the UK it is a relatively rare diagnosis with only an estimated 6000 cases/year. In the UK, 90% of cases occur in women due to the higher rate of spontaneous clearance in men.
Aetiology & pathophysiology
Trichomoniasis is caused by infection with the protozoan Trichomonas vaginalis.
T. vaginalis is a flagellated Protozoa (single-celled eukaryote) that is able to infect squamous cells of the urogenital epithelium. It most commonly infects areas of the vagina and urethra. Other sites of infection include the cervix, bladder, Bartholin glands, and prostate.
Humans are the only known reservoir for T. vaginalis and it is almost always sexually transmitted. The Protozoa can be transmitted between women and men, women and women, but rarely between two men. Co-infection with other conditions is common (e.g. rates of co-infection with bacterial vaginosis range from 20-80%).
Clinical features
Trichomoniasis classically causes a malodorous, frothy green-yellow discharge.
Symptoms
- Asymptomatic: 50% of women, 15-50% of men
- Vaginal discharge: frothy, green-yellow
- Vulval itching or soreness
- Malodorous
- Dysuria
- Urethral discharge: 20-60% of symptomatic men
- Urethral irritation
- Abdominal pain
Signs
- Women:
- Frothy green-yellow discharge
- Vulval inflammation
- Cervical inflammation (often described as ‘strawberry cervix’)
- Men:
- Usually no signs
- Rarely balanitis (inflammation of glans penis), OR
- Balanoposthitis (inflammation of glans penis and foreskin)
Diagnosis & investigations
Patients with suspected trichomoniasis should be referred to a genitourinary medicine (GUM) clinic.
Routine investigations
Women should undergo a formal assessment with speculum examination. Around 5-15% will have a normal examination. Swabs are taken from the lateral walls of the vagina for pH testing and a high vaginal swab is taken from the posterior fornix for gram staining, microscopy and culture. Alternatively, a self-taken low vaginal swab can be used for gram stain, microscopy and culture.
Vaginal pH is usually completed as part of the diagnostic work-up. An elevation in vaginal pH >4.5 is supportive of the diagnosis of trichomoniasis, but can also be seeing bacterial vaginosis (BV).
In men, a urethral swab or first void urine sample can be taken for gram stain, microscopy and culture.
STI screening
Patients being investigated for trichomoniasis should be offered STI screening to include chlamydia, gonorrhoea, syphilis and HIV. This can be organised through a sexual health or GUM clinic.
Diagnosis
Diagnosis of trichomoniasis involves identification of the protozoan from a vaginal (women) or urethral (men) sample. There are several tests that can be used to identify the organism:
- Microscopy: evidence of motile trichomonads on a wet mount slide is diagnostic. Low cost, but less accurate. Remain motile for 10-20 minutes following sample collection.
- Nucleic acid amplification test (NAAT): involves amplification of trichomoniasis genetic material (e.g. RNA) using polymerase chain reaction (PCR). Gold standard test. Can be completed on single swab or urine sample
- Rapid testing: rapid antigen tests can be used in clinics where there is limited access to microscopy, particularly in high prevalence areas. Quick turnaround of results.
- Culture: previously gold-standard before nuclear tests. Takes seven days for full culture result but highly accurate.
- Cervical cytology: trichomoniasis may be diagnosed through liquid-based cervical cytology. Could be incidental finding during cervical screening
Differential diagnosis
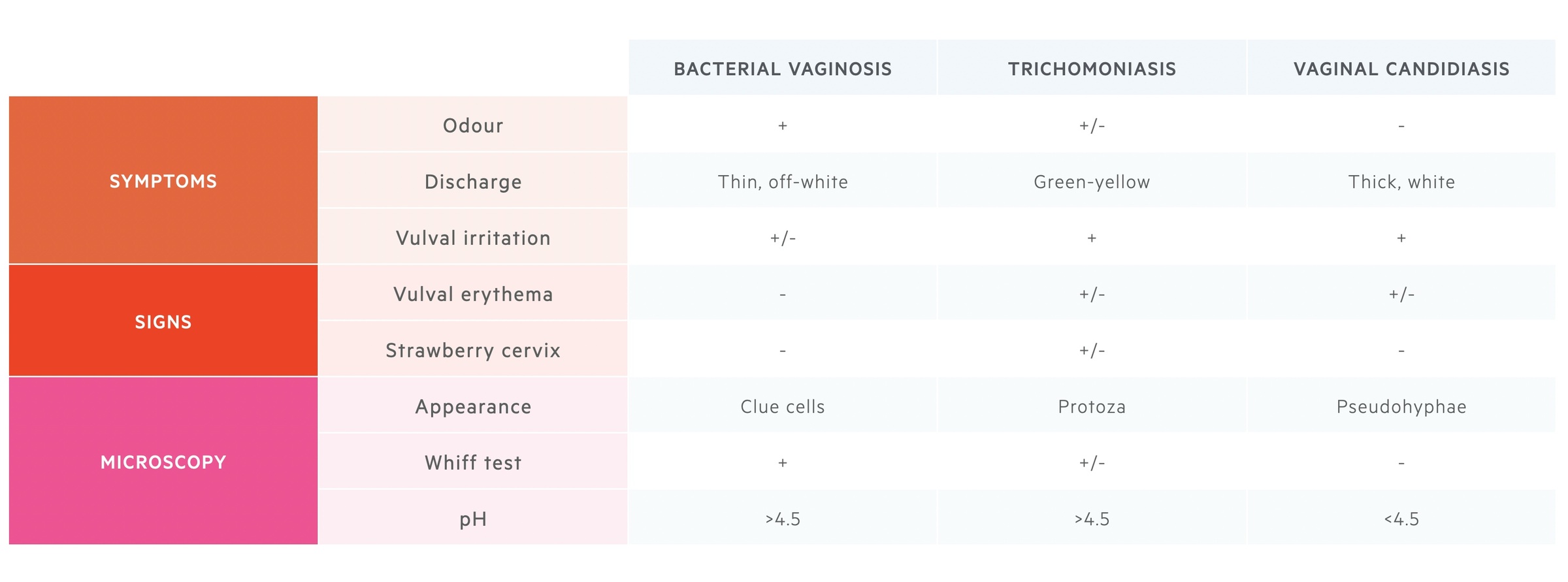
Co-infection with other conditions (e.g. BV or candidiasis) is common. Important to differentiate between candidiasis, trichomoniasis and BV, which also present with increasing vaginal discharge.
Management
Oral metronidazole is the treatment of choice in symptomatic patients.
The only reliable curative treatment of trichomoniasis is the use of 5-nitroimidazole drugs (e.g. metronidazole/tinidazole). Use of metronidazole or tinidazole has a cure rate up to 95%.
General advice
Patients need contact tracing of any recent sexual contacts. This is usually orchestrated via a GUM clinic. Any sexual partner(s) within four weeks of presentations will require empirical treatment.
Patients with trichomoniasis should be advised to engage in sexual abstinence for one week after both themselves and any partner has completed treatment.
Treatment options
The general treatment of patients with trichomoniasis is pharmacologial treatment with metronidazole as a 5-7 day course at standard dose, or a one-off, high dose. Generally, the high dose, one-off strategy is not recommended in pregnancy.
Special cases
- Reinfection: repeat treatment protocol
- Recurrent infection: if fails single dose therapy, opt for seven day course. Alternatively, consider a high dose course (e.g. metronidazole 2g daily) for seven days
- Refractory: more extensive course of 5-nitroimidazoles can be administered but this should be guided by a sexual health specialist.
Complications
Both men and women are at risk of complications associated with trichomoniasis.
Women
- Pregnancy: preterm delivery, low infant birthweight, increased risk of postpartum sepsis
- Infection: facilitate HIV transmission, increased risk of BV, pelvic inflammatory disease
- Infertility
- Malignancy: increased risk of cervical cancer
Men
- Infection: acute prostatitis, chronic prostatitis, facilitate HIV transmission
- Infertility
- Malignancy: increased risk prostate cancer
Last updated: June 2021
Further Reading
British Association for Sexual Health and HIV (BASHH) guidelines.
Have comments about these notes? Leave us feedback
