Acute stress reaction
Notes
Introduction
An acute stress reaction refers to intense, or prolonged, mental or psychological distress that can develop after exposure, or in response, to a stressful event.
Many people who experience a traumatic event will struggle with negative emotions, thoughts, and memories of the event. In the first month following the traumatic event, they may experience an acute stress reaction, symptoms of which include:
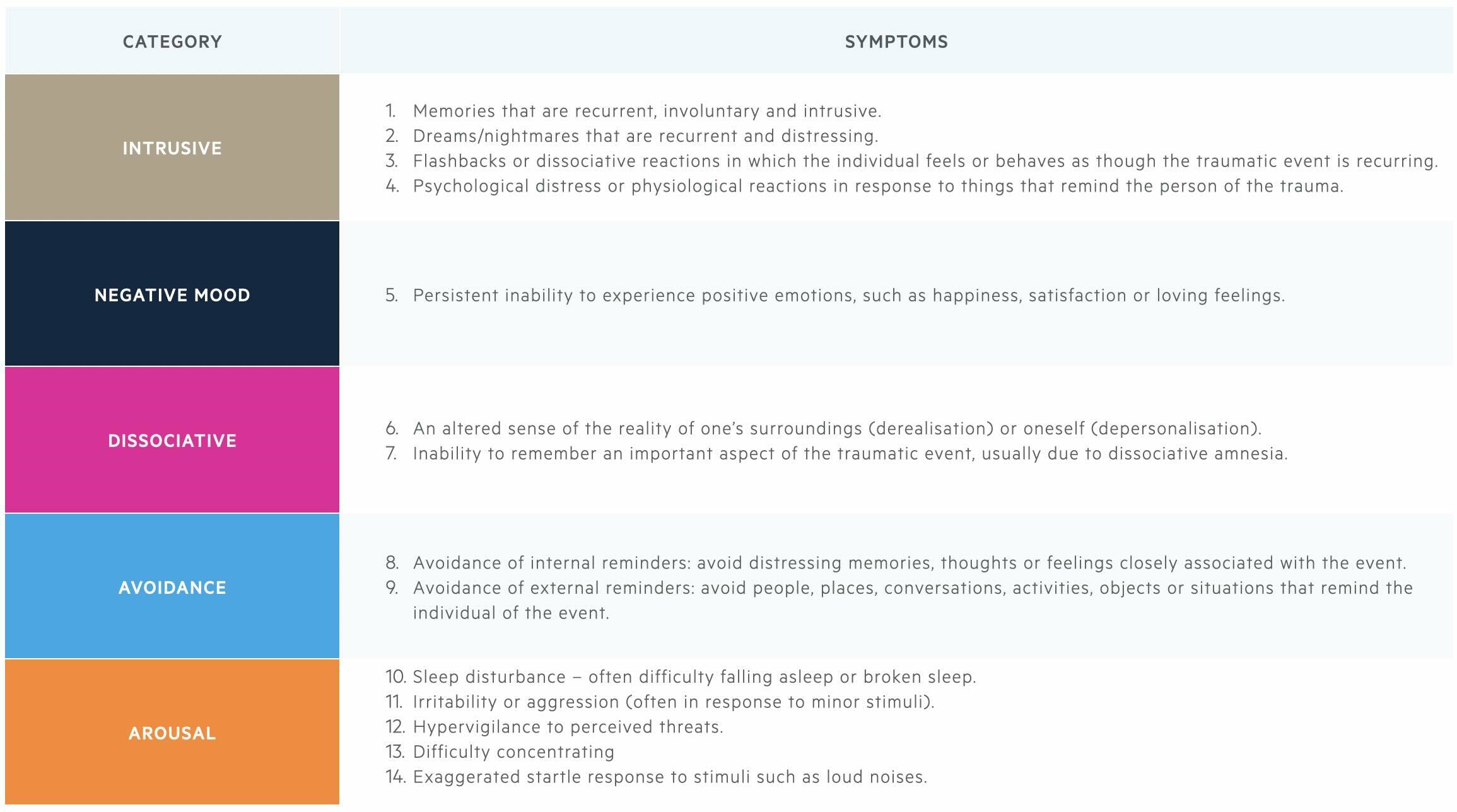
- Intrusion symptoms: reexperiencing the traumatic event (memories, flashbacks, nightmares).
- Negative mood: inability to experience positive emotions, such as happiness.
- Dissociative symptoms: an altered sense of one’s surroundings or oneself, difficulty remembering the trauma.
- Avoidance symptoms: avoidance of thoughts and memories of the traumatic event or avoidance of activities, situations, or people that remind them of the traumatic event.
- Arousal symptoms: these include an exaggerated startle response, insomnia, hypervigilance to threat, and angry outbursts.
These features develop quickly but are not long-lasting; hence acute stress reaction. Symptoms of an acute stress reaction often ease over time but for some, symptoms will persist and intensify. People who experience an acute stress reaction are at risk of going on to develop post-traumatic stress disorder (PTSD).
It is important to note that usually, mental health diagnoses can be looked at with the DSM-V and/or the ICD10 (or more recently the ICD11). In DSM-V, the above features are described by the term acute stress disorder. In ICD10 it was referred to as an acute stress reaction. ICD11 no longer considers an acute stress reaction a mental disorder, and this diagnosis has therefore been removed. The removal of acute stress reaction from ICD11 was intended to “de-pathologise” brief periods of emotional distress people experience in response to trauma. There may still be a role for identifying those experiencing an acute stress reaction as it will help detect those at a higher risk of going on to develop PTSD.
Epidemiology
The prevalence of an acute stress reaction may be up to 20%.
The prevalence of acute stress reaction/disorder is estimated to be between 5-20%. This variation is likely due to the different populations being considered, with acute stress disorder occurring more frequently in those living in conflict-affected areas. Within these areas, there is a higher likelihood of being exposed to a traumatic event. Acute stress disorder is thought to be a predictor of subsequent PTSD; however, less than half of people with acute stress disorder go on to develop PTSD.
Aetiology & risk factors
Acute stress disorder and post-traumatic stress disorder share similar risk factors.
It is thought that most risk factors for PTSD are also risk factors for acute stress disorder.
These risk factors can be divided into:
- Related to the traumatic event: increased likelihood of being exposed to a traumatic event (e.g. war zones, emergency service workers), high severity of traumatic event, experiencing the trauma directly, multiple traumas.
- Unrelated to the traumatic event: female sex, younger age, low social support, history of mental health disorder, multiple major life stressors.
Clinical features & diagnosis
Acute stress reaction/disorder is no longer recognised by the ICD11, but remains a diagnostic term in the DSM-V.
The diagnosis of an acute stress reaction differs depending on the diagnostic manual that is used to classify mental health disorders.
- DSM-V: referred to as acute stress disorder
- ICD-10: referred to as acute stress reaction
- ICD-11: no longer a recognised diagnosis*
*NOTE: The ICD11 has removed the diagnosis of acute stress reaction, intending to “de-pathologise” brief periods of emotional distress people experience in response to trauma.
DSM-V diagnostic criteria
The diagnosis of an acute stress disorder is initially dependent on exposure to trauma. This may include actual or threatened death, serious injury, or sexual violence. The person may be exposed to the traumatic event or events in one or more of the following ways:
- Directly experiencing the trauma.
- Witnessing (in person) the traumatic events occurring to others.
- Learning that the traumatic events occurred to a close family member or friend.
- Experiencing repeated or extreme exposure to unpleasant details of the traumatic event (for example first responders to a road traffic accident).
The presence of nine or more of the following 14 symptoms from the below 5 categories is consistent with the diagnosis of acute stress disorder:
- Intrusion symptoms
- Negative mood
- Dissociative symptoms
- Avoidance symptoms
- Arousal symptoms
The above symptoms typically:
- Begin immediately after the trauma and duration is from 3 days – 1 month.
- Cause the individual significant distress or functional impairment (social, occupational, or other important aspects of functioning).
- Cannot be better explained by another illness, substance use, or medication.
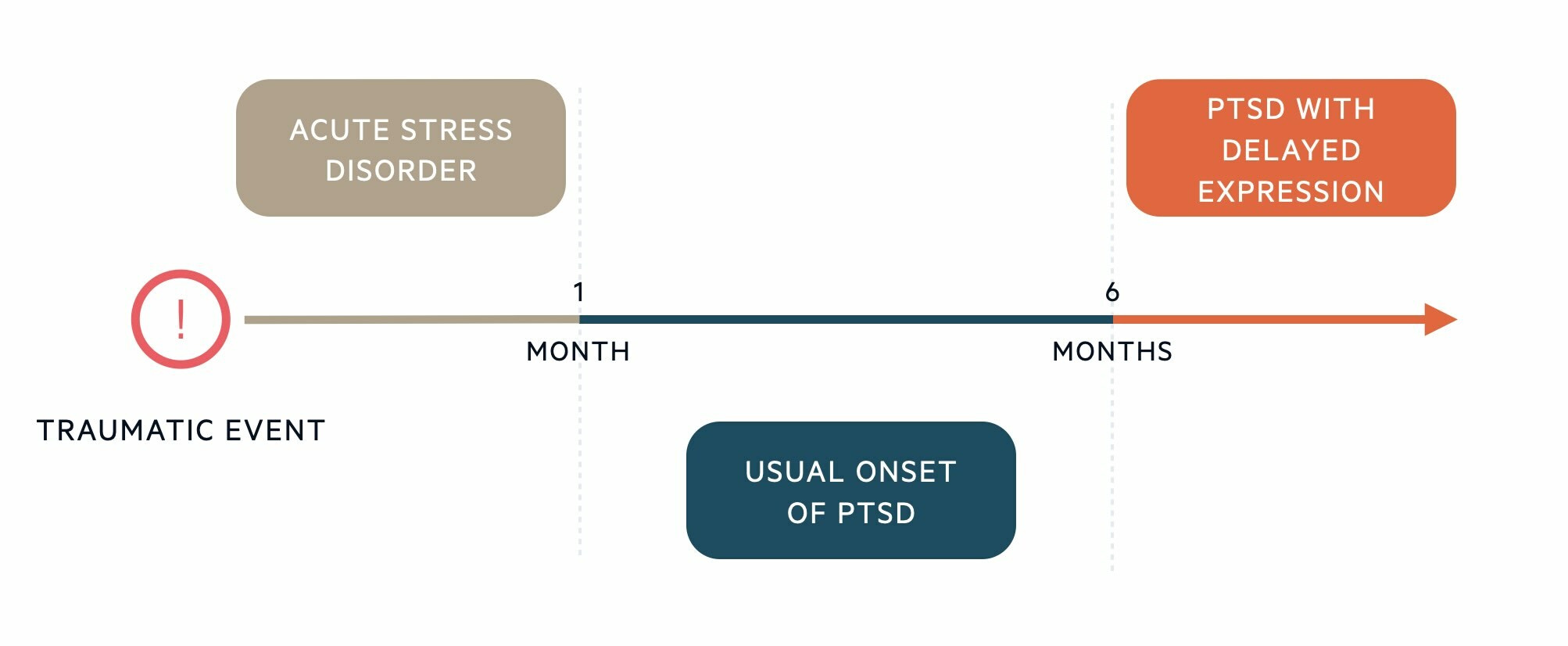
Diagnostic timeline
The clinical features of acute stress disorder and PTSD have significant overlap. The key differentiator is the timeline of these disorders (i.e. when the symptoms occur in relation to the traumatic event and the symptom duration).
- Acute stress disorder
- Symptom onset: Typically begins immediately or within a few days of the traumatic event.
- Minimum duration of symptoms: 3 days
- Maximum duration of symptoms: 1 month
- Post-traumatic stress disorder
- Symptom onset: May begin soon after the traumatic event and usually within 6 months of the trauma*
- Minimum duration of symptoms: 1 month
- Maximum duration of symptoms: none
*NOTE: If the full diagnostic criteria for PTSD are not met until at least 6 months after the event, then the DSM-V refers to this as PTSD with delayed expression.
Differential diagnosis
Post-traumatic stress disorder is the main differential of an acute stress reaction that shares the same clinical features.
- PTSD: the clinical features of an acute stress disorder and PTSD have significant overlap. The key differentiator is the timeline of symptoms from the traumatic event (detailed above).
- Adjustment disorder: this is similar, in that emotional and behavioural symptoms develop in response to an identifiable stressor. However, the stressor is usually less severe. The distress experienced in adjustment disorder is disproportionate to the severity of the stressor.
- Depression: common features include low mood, inability to experience positive emotions, loss of interest/enjoyment in activities, negative beliefs about oneself, irritability, sleep disturbance, and poor concentration.
- Anxiety disorders: including generalised anxiety disorder, panic disorder, and specific phobias. Acute stress disorder shares several features with anxiety disorders including poor concentration, irritability, and avoidance of situations that trigger anxiety.
- Dissociative disorders: characterised by depersonalisation (feeling detached from oneself) and derealisation (feeling detached from surroundings).
- Psychosis: vivid intrusive flashbacks or memories of the traumatic event may be difficult to distinguish from hallucinations. The key differentiator is that psychosis is characterised by a loss of contact with reality whereas with features of PTSD reality testing remains intact.
Management
A watch-and-wait strategy is usually preferred due to the time-limited nature of an acute stress reaction.
Given the time-limited nature of an acute stress reaction, often no treatment is required or offered. Clinicians usually take a watch-and-wait approach with active monitoring. Symptoms of an acute stress reaction often ease over time but for some, symptoms will persist and intensify. If those who initially experience an acute stress reaction go on to develop PTSD, they may benefit from talking therapies and/or medications.
There may be some benefit of trauma-focused cognitive behavioural therapy in those experiencing an acute stress reaction, as this aims to minimise symptom severity and reduce the likelihood of an individual developing PTSD. This is not routinely offered on the NHS for those experiencing an acute stress reaction but is a key psychological therapy used in the management of PTSD.
Psychological-focused de-briefing after the traumatic event is not recommended as it is thought to show no benefit and evidence suggests that individuals may have worse outcomes than those who receive no treatment. Psychological debriefing involves encouraging individuals to recall the traumatic event and process their thoughts and emotions surrounding what happened, either in a group or individual setting.
Medication would not be routinely advised in the management of an acute stress reaction. If the individual is struggling with their sleep, they may benefit from a short course of a hypnotic medication (e.g. zopiclone).
As with other mental health disorders, the following points form an important part of any management plan and should be considered:
- Inform and educate the patient about the disorder.
- Involve family members or support network.
- Assess and manage risk – the individual may pose a risk of harm to themselves or others. Those deemed to have risks may require more intensive support and monitoring (home treatment team, inpatient admission).
- Assess for and provide appropriate treatment for commonly co-occurring mental health disorders including depression, anxiety, and substance or alcohol misuse.
- Assess the person’s physical health.
- Assess the person’s social needs.
Last updated: December 2023
References:
DSM-V
ICD-10
ICD-11
NICE guidelines for PTSD - Overview | Post-traumatic stress disorder | Guidance | NICE
Have comments about these notes? Leave us feedback
