Social anxiety disorder
Notes
Introduction
In social anxiety disorder, the fear of social situations is overwhelming and disproportionate.
It is normal to feel nervous in some social situations, such as attending a job interview or going on a date. However, in social anxiety disorder, the fear of social situations is overwhelming and disproportionate. The individual is fearful of being negatively judged by others in a variety of social settings including everyday social interactions, being observed by others, and performing in front of others. There may be a fear of humiliation, embarrassment, or social rejection. Individuals with social anxiety disorder therefore strive to avoid these social situations or endure them with intense feelings of anxiety or fear. This avoidance can harm an individual’s day-to-day life, including their ability to work or attend school, their relationships, and their daily routines.
We will explore the features of social anxiety disorder in detail in the diagnosis section below. We have focussed on the diagnosis and treatment of social anxiety disorder in adults, however many of the same principles apply in children and adolescents.
Epidemiology
It is estimated that up to 15% of adults may have social anxiety disorder during their lifetime.
Studies have shown that 8-15% of adults will have social anxiety disorder at some point in their lives. The median age of onset is 13 years and it is one of the most persistent anxiety disorders. Social anxiety disorder more commonly affects women than men. There is significant comorbidity between social anxiety disorder and other mental health problems including depression (19%) and substance use disorder (17%).
Aetiology & risk factors
The aetiology of most anxiety disorders is thought to be a complex interaction between environmental factors, genetic factors, and psychological traits of an individual.
The amygdala is an area of the brain, that plays a role in the fear response. There is evidence to suggest that those with an overactive amygdala have a heightened fear response which contributes to increased levels of anxiety in social situations.
The risk factors for the development of social anxiety disorder include:
- Female sex
- Family history of an anxiety disorder: anxiety disorders tend to run in families but it isn’t clear how much of this is related to genetics versus learned behaviour.
- Adverse childhood experiences (e.g. parental death, maltreatment or abuse, bullying).
- Overprotection from primary caregivers in childhood.
- Shy and/or timid temperament.
- Embarrassing situations: social anxiety disorder may develop after experiencing a distressing or embarrassing social situation.
- Noticeable condition(s): may make an individual more self-conscious and trigger anxiety in social situations.
- Other mental health disorders (e.g. other anxiety disorders, depression).
Clinical features & diagnosis
The DSM-V refers to a clinical diagnosis of social anxiety disorder, whereas the ICD-11 refers to social phobia.
Both DSM-V and ICD-11 can be used as frameworks to aid the clinical diagnosis of social anxiety disorder. In DSM-V it is called social anxiety disorder and in ICD-11 it is called social phobia.
The diagnosis of social anxiety disorder is outlined using DSM-V criteria, which is listed below:
In social anxiety disorder, there is fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. These situations include:
- Social interactions (e.g. having a conversation, meeting unfamiliar people).
- Being observed whilst doing something (e.g. eating or drinking in the presence of others).
- Performing in front of others (e.g. giving a speech).
Fear of judgement - the individual fears that they will act in a way or show anxiety symptoms that will be negatively evaluated by others (fear of humiliation, embarrassment, rejection by others, or causing offense to others)
The fear or anxiety is:
- Almost always provoked by the social situations.
- Disproportionate to the actual threat posed by the social situation.
The social situations are:
- Actively avoided OR
- Endured with intense fear or anxiety.
The fear, anxiety, or avoidance behaviours are:
- Persistent, lasting for >6 months.
- Cause the individual significant distress or functional impairment (social, occupational, or other important aspects of functioning).
- Not better explained by another mental disorder, medical condition, or effects of a substance.
Differential diagnosis
The main differentials for social anxiety disorder are another anxiety disorder, OCD, or autism spectrum disorder.
- Generalised anxiety disorder: excessive anxiety about several events and activities, not limited to the situations and anxieties that characterise social anxiety disorder.
- Specific phobia: if fear, anxiety and avoidance behaviour are related to something other than the fear of being negatively judged by others in social situations, then they may have a different specific phobia (e.g. fear of enclosed spaces).
- Panic disorder: if panic attacks occur in the context of social anxiety disorder they tend to be predictable and occur in social situations. In panic disorder, panic attacks are unexpected with no clear trigger.
- Body dysmorphic disorder (BDD): in BDD the individual may avoid social situations, but this anxiety and avoidance behaviour is driven by perceived flaws in physical appearance.
- Obsessive-compulsive disorder (OCD): disproportionate anxiety and avoidance behaviours can be seen in OCD, for example, obsessions about contamination may drive compulsive behaviour to avoid some social situations deemed to be high risk for contamination.
- Autism spectrum disorder (ASD): ASD may predispose an individual to social anxiety due to a deficit in social communication and social interactions.
Management
Social anxiety disorder can be treated with talking therapies, medication or a combination.
The two major management strategies in social anxiety disorder include talking therapies and pharmacotherapy. Decisions around treatment will be guided by the severity of the presentation and patient preference. For those with social anxiety disorder that only results in mild to moderate functional impairment, psychotherapy is usually the first-line option. For social anxiety disorder that has a more severe impact on an individual’s functioning, they are likely to benefit from a combination of psychotherapy and medication.
Psychological therapies
Three major psychological therapies may be used in social anxiety disorder:
- Self-help therapy
- Cognitive behavioural therapy: individual and group
- Psychodynamic therapy
A patient with less severe functional impairment may opt to try guided self-help for the management of social anxiety disorder. This involves working through a cognitive behavioural therapy (CBT)-based workbook with or without support from a therapist.
Those patients with more severe functional impairment are likely to benefit from a course of individual CBT. This usually consists of 15 one-hour-long sessions with a therapist over 4 months.
Group CBT is sometimes offered but is deemed to be less effective than individual CBT for those with social anxiety disorder.
Adults who decline CBT and pharmacological intervention may be offered short-term psychodynamic psychotherapy. This is thought to be less clinically effective and less cost-effective when compared to CBT, self-help and pharmacological interventions. This usually consists of 25-30 sessions of 50 minutes duration over 6-8 months.
Cognitive Behavioural Therapy
Cognitive Behavioural Therapy (CBT) focuses on the link between our thoughts, behaviours and emotions. Challenging negative thoughts and changing unhelpful behaviours can have a positive impact on how a person feels. The cognitive component of CBT for social anxiety disorder might involve challenging negative automatic thoughts, beliefs or expectations of going to feared social situations.
The behavioural component of CBT for social anxiety disorder involves exposure therapy – the individual is supported to gradually expose themselves to the social situations that are feared and usually avoided. This is called systematic desensitisation which is a commonly used CBT method for the treatment of phobias. It involves working with a therapist to construct an anxiety “hierarchy” that ranks situations that cause anxiety from the least to the most anxiety-inducing.
Please see the example anxiety hierarchy for social anxiety disorder related to fear of public speaking:
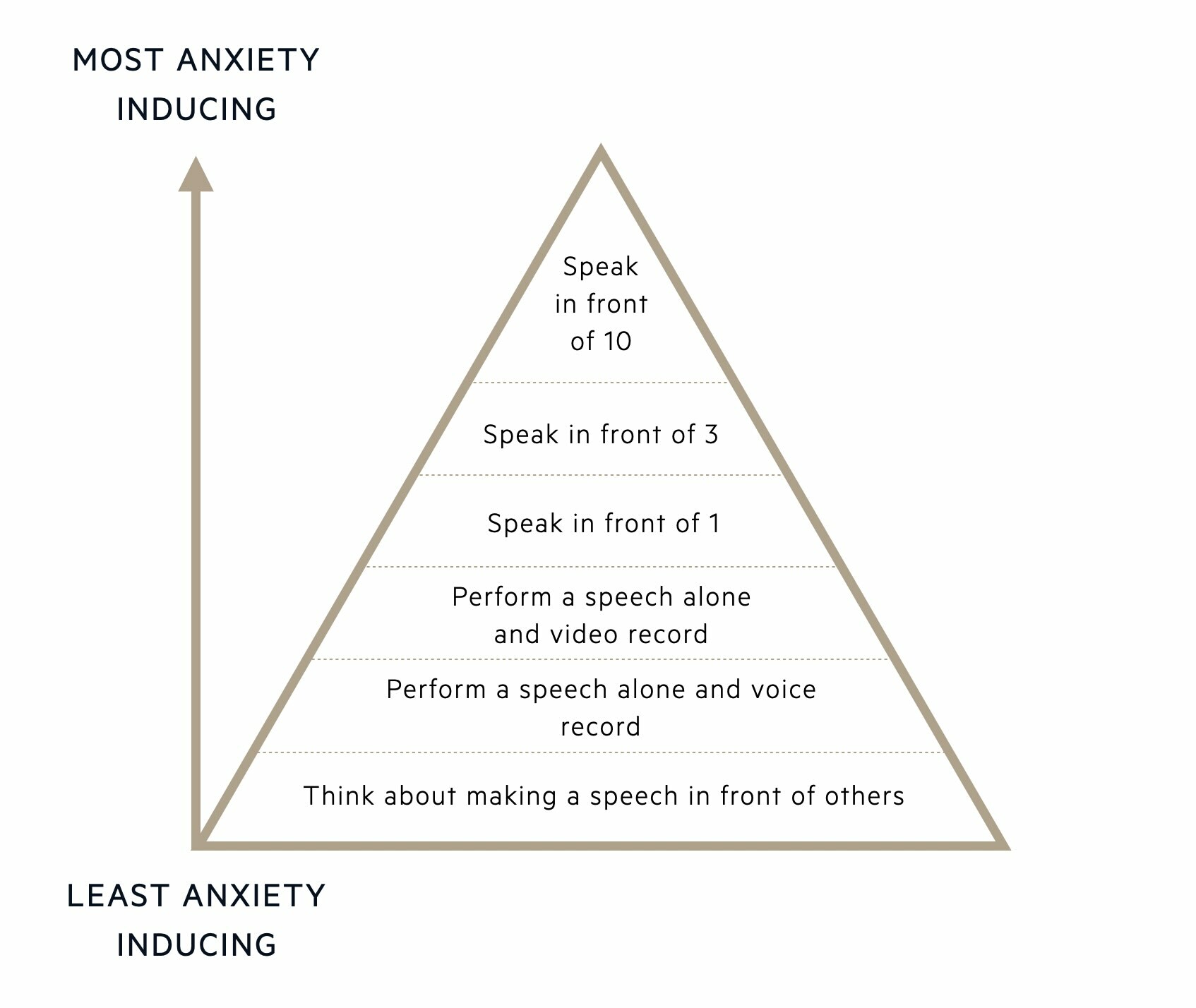
The individual will be supported by the therapist to gradually work their way up the anxiety hierarchy, starting by exposing themselves to situations that cause the least anxiety and finishing with exposure to the most anxiety-inducing situations. The therapist also teaches the individual relaxation techniques to help manage anxiety at each stage of the hierarchy. By gradually exposing themselves to more stressful situations, using relaxation techniques and tolerating the anxiety, the fear response should over time reduce. The aim is to reduce the fear response to social situations and replace this with a relaxation response.
Psychodynamic psychotherapy
Psychodynamic psychotherapy looks at how a person’s life experiences affect their thoughts, feelings, behaviours and how they interact with others. Developing a secure positive therapeutic alliance between the patient and therapist is key in psychodynamic psychotherapy. Negative beliefs about relationships and themselves can be challenged and social skills improved.
Pharmacotherapy
The three major classes of drugs that can be used in social anxiety disorder include:
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin-noradrenaline reuptake inhibitors (SNRIs)
- Monoamine oxidase inhibitors (MAOIs)
Below is the flow chart for the pharmacological management of social anxiety disorder, as per the NICE Guidelines:
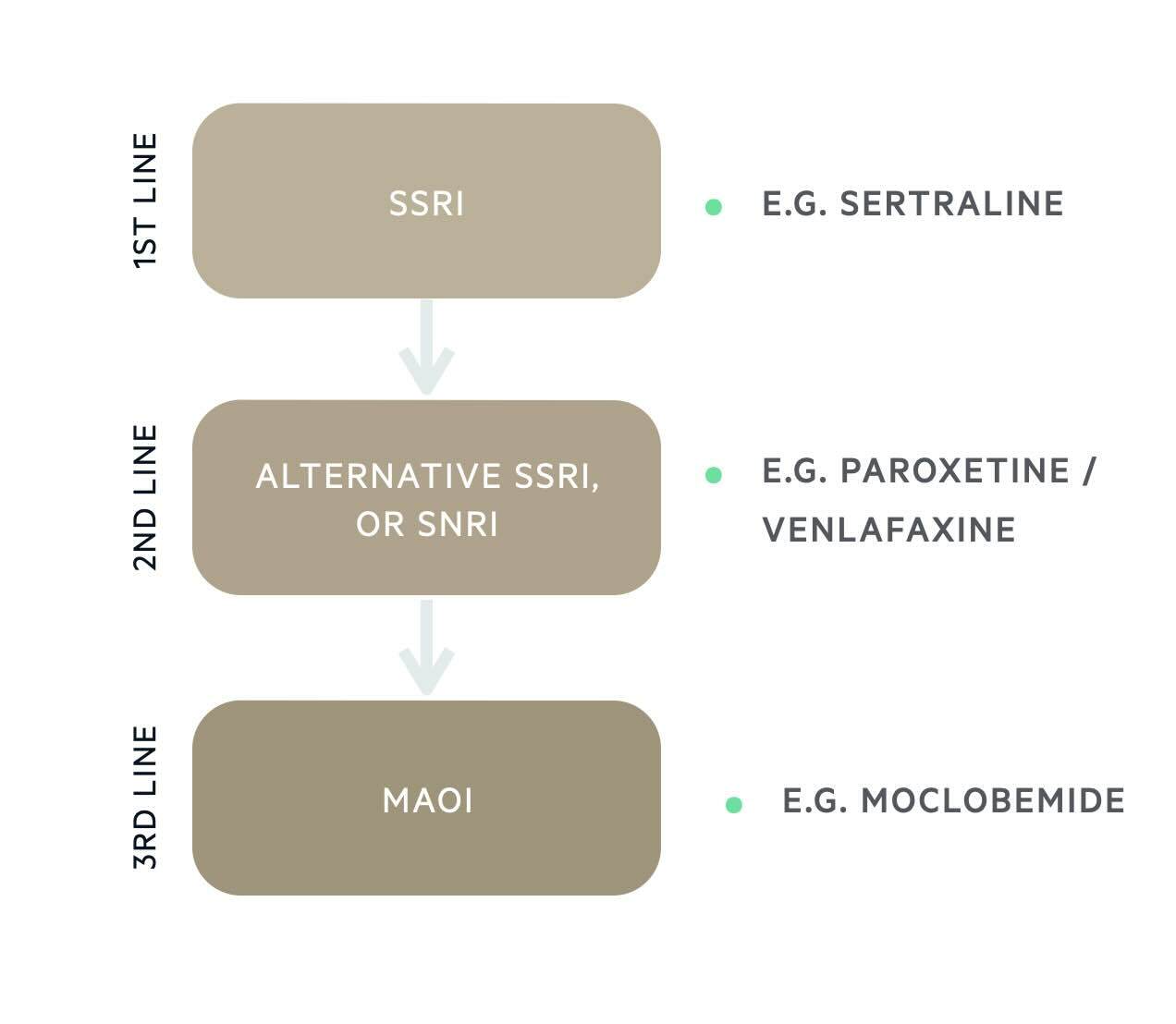
It is not necessary to remember the specific medications licensed for social anxiety disorder, but it is useful to be aware of the general principles, as this is similar to the treatment of most anxiety disorders with use of an SSRI first line, a different SSRI or SNRI second line, and specialist referral third line for others therapies (e.g. MAOI).
Principles of prescribing SSRIs and SNRIs
Before starting an SSRI or SNRI it is important that you:
- Explain the likely benefits.
- Advise patients when they might start experiencing anxiolytic effects: 2 weeks.
- Advise patients what the likely treatment duration is: at least 6 months.
- Inform about possible side effects (including a transient increase in anxiety).
- Advise patient not to cease medication abruptly: there is a risk of discontinuation syndrome and relapse in symptoms.
For individuals <30 years old who are starting an SSRI or SNRI, it is important to:
- Warn them there is an association with an increased risk of suicidal thinking and self-harm.
- Review within 1 week of prescribing.
- Continue to monitor the risk of suicide and self-harm every week for the first month.
Monitoring patients on SSRIs and SNRIs is important and should include monitoring of:
- Therapeutic response: takes 2 or more weeks for anxiolytic effect.
- Side effects: GI disturbance (loss of appetite, nausea, abdominal pain, diarrhoea, constipation), headaches, poor sleep, transient increase in anxiety, palpitations, sexual dysfunction (loss of libido, erectile dysfunction, inability to orgasm).
- Advise them to remain on SSRI for at least 6 months after remission of symptoms: chance of relapse is high if medication is discontinued abruptly.
Other management considerations
As with other mental health disorders, the following points also form an important part of any management plan and should be considered:
- Explain & educate: written information on social anxiety disorder and treatment options (psychotherapy and medication) is often helpful. It may be hard for the patient to retain information given verbally. It can also be helpful to give lifestyle advice that can help manage anxiety including exercising regularly, eating a healthy diet, avoiding caffeinated drinks, and avoiding alcohol consumption.
- Involve the support network: the family may benefit from practical or emotional support and education about the disorder.
- Assess and manage risk: those deemed to be high risk to themselves may require more intensive support and monitoring (home treatment team, inpatient admission).
- Active monitoring: the management plan may need to change if the individual’s presentation or risks change.
- Screen for co-morbidities: assess for and provide appropriate treatment for commonly co-occurring mental health disorders including other anxiety disorders and depression.
- Screen for substance or alcohol misuse: alcohol and drug misuse is often an attempt to reduce anxiety in social situations. The patient may benefit from additional input from drug and alcohol services.
Last updated: January 2024
References:
DSM-V
ICD-11
NICE Clinical guideline [CG159] - Social anxiety disorder (nice.org.uk)
Have comments about these notes? Leave us feedback
