Substance use disorders
Notes
Introduction
Substance abuse or misuse is a repetitive harmful pattern of substance use that leads to negative consequences
Substance abuse is a major problem both in the UK and more broadly across the world. Common substances of abuse, which can lead to dependence, include alcohol, opioids, cocaine, and a variety of legal substances such as nicotine and caffeine. In this article, we go over the general principles for substance misuse. For more specific information regarding a single substance, please see the relevant notes in our Psychiatry section.
Substance abuse or misuse
Substance abuse or misuse is a repetitive harmful pattern of substance use that leads to negative consequences (e.g. relationship issues, work problems, getting into risky situations). The misused substance can be legal or illegal. Legal substance misuse means that the substance is taken in a way or for a purpose not consistent with medical or legal guidelines.
Substance dependence
Substance abuse or misuse can lead to more severe substance dependence, which is characterised by:
- Craving the substance: this is experienced as a strong desire or compulsion to use the substance.
- Loss of control over substance use.
- Tolerance: reduced effects of a substance after repeated use. This means increased doses are needed to feel the desired effects.
- Withdrawal symptoms: these occur when substance use is ceased or reduced. Usually manifests as unpleasant possibly dangerous physical and psychological symptoms.
- Prioritisation: substance use takes priority and other important activities/interests are neglected.
- Persistent substance use despite harmful consequences.
Substance Use Disorder
The diagnosis of Substance Use Disorder, introduced by the DSM-V, encapsulates a spectrum of disorders that can range from a few features of substance misuse/abuse with minimal impact on functioning, to more severe substance dependence.
Epidemiology
The prevalence of substance misuse and dependence varies with age, sex, and employment status (more common in the unemployed).
It is estimated that 9% of adults aged 16 to 59 have taken illicit drugs in the last year. Of this age group, 3.5% have taken a Class A drug. Approximately 20% of young adults (16-24 years) are thought to have taken illicit drugs in the last year.
Drug dependence is more common in men than women (2:1). Drug dependence is most common in men aged 16-24 years (11.8%). More than two-thirds of people in treatment for substance misuse are men. Of those adults under drug and alcohol services for opioid treatment, 72% are men. Of those adults under drug and alcohol services for treatment of alcohol misuse, 58% are men and 42% women.
The two major substances of abuse among adults are opioids and alcohol. Of the adults in treatment for substance misuse, 51% are being treated for opioid dependence and 28% for alcohol dependence.
Aetiology and risk factors
Multiple factors contribute to increased risk of developing substance use disorders.
Risk factors for substance abuse and misuse include:
- Family history of substance misuse and genetic factors.
- Social and environmental factors: poor school achievement, unemployment, social deprivation, history of criminal activity, peer influence, and normalisation of substance misuse in the individual’s culture or peer group.
- Adverse life events: stressful life events may trigger substance misuse.
- Drug-related factors: availability and affordability of the substance, early use of drugs, and taking a drug that has a high propensity to lead to physical and psychological dependence.
- Personality traits: including disinhibition, poor impulse control, novelty or sensation seeking may increase the risk of substance misuse.
- Psychiatric co-morbidities (depression, anxiety, PTSD, psychosis): illicit drugs may be used in an attempt to self-medicate.
Taking a substance misuse history
It is important to screen patients regarding substance misuse in clinical practice.
Substance misuse can take many forms including the use of alcohol, tobacco, or illicit drugs. It is important to screen for and ask directly about substance misuse. The individual may not acknowledge substance use unless this is directly asked in a non-judgmental way.
Common substances that might be asked about within a medical history include:
- Alcohol
- Tobacco
- Cannabis
- Opioids (e.g. methadone, heroin)
- Stimulants (e.g. cocaine, amphetamines, ecstasy/MDMA)
- Sedatives (e.g. benzodiazepines, Z-drugs)
- Hallucinogens (e.g. LSD, psilocybin)
For each identified substance, it is important to ask for further details about the use of that substance. This can include:
- Quantity used.
- Frequency of use.
- Pattern of use (e.g. socially, alone, in certain environments).
- When the substance was last used (i.e. are they at risk of withdrawal).
- Total duration of use.
- Route of use (e.g. smoked, oral, snorted, injected).
- How substance is obtained.
NOTE: when discussing the route of administration, be sure to ask about (and promote) safe needle practices in the context of injecting drugs.
DSM-V criteria for Substance Use Disorder
When discussing substance use within the medical history, try to explore areas that relate to the DSM-V criteria for Substance Use Disorders. Think about how the patients' answers relate to these criteria as they will help make a formal diagnosis.
- Increased consumption of the substance: either taken in larger amounts or over longer periods than intended.
- Loss of control of substance use: inability to control when the substance is used, how much is used, or unsuccessful attempts to stop substance use.
- Craving the substance: a strong desire or compulsion to take the substance.
- Substance use is time-consuming: aka spending a lot of time obtaining, using, or recovering from the substance.
- Increased tolerance to substance: needing more of the substance to produce the desired effect.
- Withdrawal symptoms: developing symptoms of withdrawal upon cessation of the substance or avoiding withdrawal symptoms by continued substance use.
- Prioritisation: substance use takes priority and other important activities/interests are neglected (social, occupational, or recreational).
- Continued substance use: this is despite harmful consequences to physical health, mental health, relationships, and inability to fulfill responsibilities.
Always ask about past contact with drug and alcohol treatment services, including previous efforts to reduce/stop drug use.
Other aspects of the medical history
Assess for physical health problems associated with substance misuse (e.g. chronic lung disease from smoking).
Assess for mental health problems associated with substance misuse (e.g. depression, anxiety), and ask about previous contact with mental health services.
Assess for social problems associated with substance misuse. This might include unemployment, crime, previous imprisonment, involvement in the sex industry, homelessness, child protection issues, or domestic abuse.
Ask about any family history of substance use and/or dependence.
Risk assessment
It is important to conduct a thorough risk assessment when dealing with substance misuse:
- Risks associated with injecting drugs: ask where the individual gets their supply of needles. Ask about needle-sharing habits. Ask about whether used injecting equipment is disposed of correctly. Ascertain whether they have had screening for blood-borne viruses. Ask about safe sex practices.
- Risk of deliberate self-harm or suicide: mental health issues are common in those who misuse drugs and it is important to consider the risk the individual may pose to themselves. Ask about a history of self-harm and suicidal acts. Assess for current thoughts of self-harm and suicide. Assess for suicidal intent or plan.
- Risk to others: the individual may act erratically or aggressively when intoxicated. The risk of harm to dependents/children needs to be considered including child neglect (being intoxicated when caring for children, being unable to meet their needs, leaving children unsupervised), or other forms of child abuse. It is important to consider how the substance is being stored and whether children may have access to it.
- Risk from others: being intoxicated can make individuals more vulnerable to harm from others. Substance intoxication may also increase risky behaviours or increase exposure to risky situations. Individuals may go to extreme lengths and do unsafe things to obtain drugs (e.g. stealing, sex work).
Assess the individual’s insight into the nature and extent of harm caused by substance misuse. Finally, assess their readiness/motivation for change.
Physical examination
A physical examination is essential in the presence of substance misuse due to the risks associated with intoxication and withdrawal.
General poor health, malnutrition, and self-neglect are common among those with substance misuse.
Weight loss, dental disease, and unexplained bruises/injuries are common in those with substance misuse. It is important to assess for more substance-specific signs and underlying physical complications. For example, physical signs and complications of prolonged excess alcohol consumption may include facial redness, spider veins, jaundice, peripheral neuropathy, unsteadiness on feet, and cognitive impairment.
In this regard, look for signs of acute intoxication (e.g. confusion) or signs of withdrawal (e.g. tremor, sweating, anxiety).
Assess for signs of injecting and associated complications. Physical health complications secondary to injecting substances include:
- Infection: introduced into the body by unsterile injection practices. Common pathogens include Staphylococcus aureus or Group A Streptococci. Infections can be localised to the injection site (skin/soft tissue infection, abscess) or spread systemically (e.g. bacterial endocarditis, osteomyelitis, sepsis).
- Blood-borne viruses: HIV, hepatitis B, and hepatitis C.
- Deep vein thrombosis and pulmonary emboli: injecting drugs increases the risk of superficial thrombophlebitis due to repetitive trauma, unsterilised techniques, and irritation caused by drug mixtures. Individuals who inject drugs are at a substantially higher risk of developing a DVT.
- Other lower limb complications: the veins in the groin are commonly used sites for drug injection. This can lead to leg ulcers, varicose veins, and chronic leg swelling.
Investigations into substance misuse
Urine samples are commonly used as part of a screen to detect for substance misuse.
Urine samples may be part of the initial assessment when drug use is suspected or for monitoring of individuals attending detoxification programmes. The time that drugs can be detected in urine depends on multiple factors including drug type, the amount consumed and biological factors for each person. Different drugs persist in urine for different lengths of time.
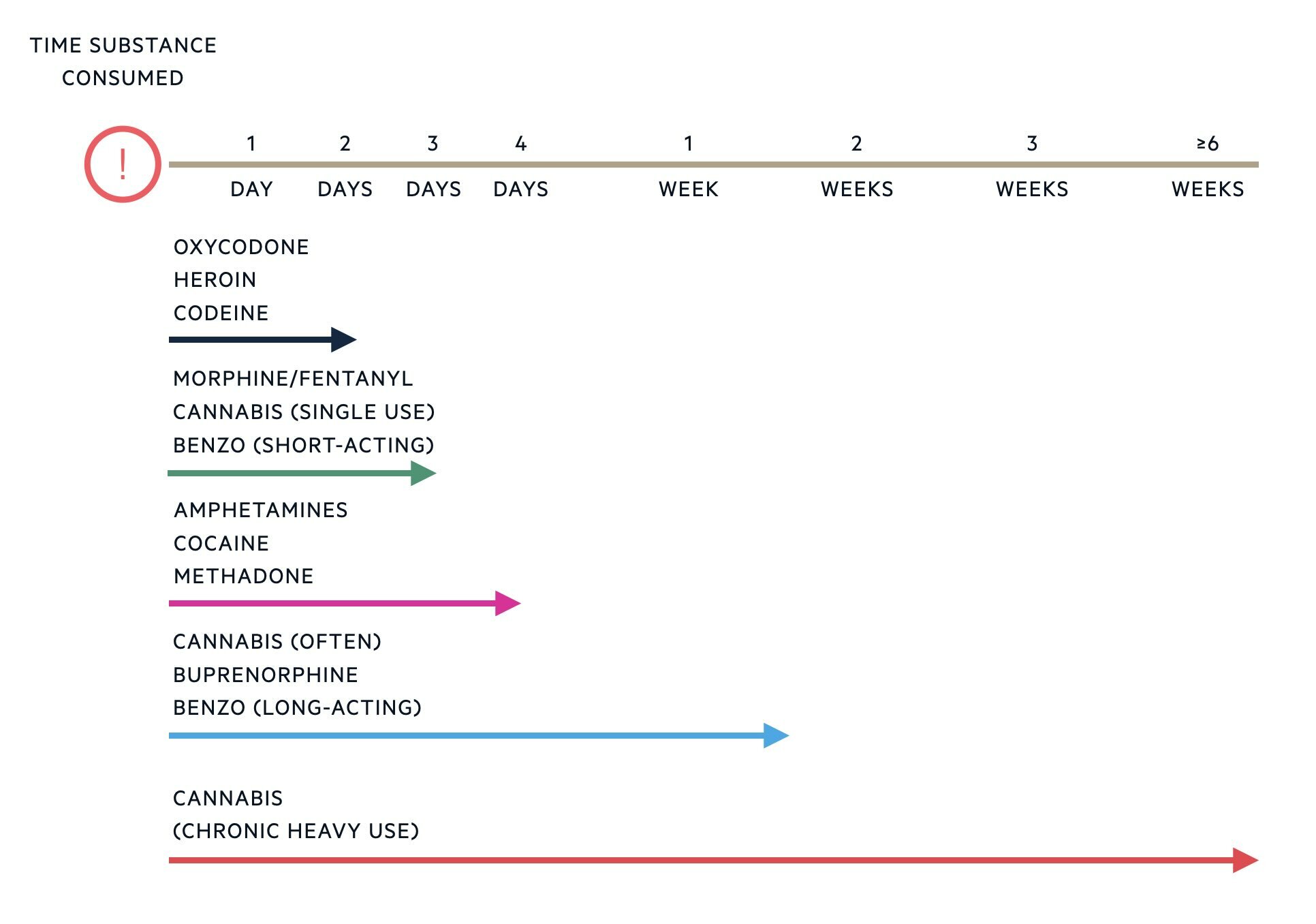
There may be attempts to substitute or dilute urine to pass urine drug tests. Clinicians can check that the provided urine sample is valid by testing the specific gravity, pH, creatinine and temperature.
Other investigations include:
- Screening for blood-borne viruses (HIV, hepatitis B and C).
- Screen for sexually transmitted infections: if concern regarding high-risk behaviours.
- Full blood count: if concern regarding anaemia or infection.
- Liver function and renal function: drugs may alter liver or renal function. Many drugs are also metabolised in the liver and excreted via the kidneys.
- Vitamin B12, folate and iron: if nutritional deficiency is suspected.
- High cardiovascular risk: HbA1c or fasting glucose, and cholesterol.
- Consider the need for an ECG: methadone and cocaine can both increase the QTc interval and subsequently increase the risk of ventricular arrhythmias. Amphetamine and cocaine use can cause tachycardia. Additionally, cocaine is known to induce coronary spasm and increase the risk of thrombus formation which can lead to myocardial ischaemia or infarction.
Diagnosis of substance related disorders
The diagnosis of Substance Use Disorder is based on the DSM-V.
In the DSM-V chapter detailing substance-related disorders, these are initially categorised by the class of drug:
- Alcohol
- Caffeine
- Cannabis
- Hallucinogens
- Inhalants
- Opioids
- Sedatives, hypnotics and anxiolytics
- Stimulants
- Tobacco
- Other (or unknown) substances
Specific substance-related disorders are further divided into:
- Substance use disorders
- Substance-induced disorders: this includes intoxication, withdrawal, and other substance-induced mental disorders (e.g. psychosis, depressive disorders).
In the DSM-IV, substance abuse and substance dependence were separate diagnoses. However, the DSM-V has merged these diagnoses and they are now encompassed by the diagnosis of 'Substance Use Disorder'.
A diagnosis of Substance Use Disorder is made when it meets the following DSM-V criteria and is substance-specific (e.g. related to opioids, alcohol, or cannabis).
DSM-V criteria - Substance Use Disorder
A problematic pattern of substance use leading to clinically significant impairment or distress.
At least 2 of the following, occurring within a 12-month period:
- Increased consumption: a substance is often taken in larger amounts or over longer periods than intended.
- Loss of control: persistent desire or unsuccessful efforts to cut down or control substance use.
- Time-consuming: a lot of time spent in activities necessary to obtain the substance, use the substance, or recover from its effects.
- Craving: a strong desire or urge to use the substance.
- Not fulfilling responsibilities: recurrent substance use causes failure to fulfill major role obligations at work, school, or home.
- Continued substance use despite negative effects on social or interpersonal problems: these problems are likely to have been caused or exacerbated by the substance effects.
- Substance use takes priority over other activities: important social, occupational, or recreational activities are given up or reduced because of substance use.
- Recurrent substance misuse in situations in which it is physically hazardous.
- Continued substance use despite negative effects on physical or mental health.
- Tolerance: a need for increased amounts of the substance to achieve intoxication or diminished effects with continued use of the same amount of the substance.
- Withdrawal symptoms: symptoms of withdrawal upon ceasing substance use, or avoiding the effects of withdrawal by continuing substance use.
Severity specifiers for substance use disorder are:
- Mild = 2 to 3 symptoms
- Moderate = 4 to 5 symptoms
- Severe = 6 or more symptoms
NOTE: Addiction is not used as a diagnostic term in DSM-V, but it is commonly used in clinical practice to describe severe problems related to compulsive and habitual use of substances. Substance Use Disorder is the chosen term, as it is thought to be more neutral and can be used to describe mild and more severe forms of the disorder.
Management
The management of substance misuse, abuse, and dependence is complex and involves a full multidisciplinary approach.
The following treatment considerations are important for the management of substance use disorders:
Multidisciplinary team
Several members of the multidisciplinary team may be involved in patients with substance misuse and dependence including a specialist Community Drug and Alcohol Team, GP, psychiatrist, and social worker.
Psychoeducation
Patients (known as clients) should be given psychoeducation on substance misuse, and encouraging positive behaviour change with motivational interviewing.
This involves the clinician adopting a supportive collaborative approach to the client, that aims to strengthen the individual’s own motivation and commitment to change. This allows the individual to identify their reasons for change based on their values and interests. Individuals should also be considered for referral to psychological therapies that focus specifically on substance-related issues.
Social support
Individuals should be encouraged to attend or engage with support groups (Alcoholics Anonymous, Narcotics Anonymous, SMART Recovery). It is also important to address social problems that may be associated with substance misuse including unemployment, crime, involvement in the sex industry, and/or homelessness. Support from families and carers, where possible, is essential to long-term recovery.
Managing intoxication and withdrawal
Management needs to focus on addressing both the effects of intoxication and withdrawal, which can be life-threatening (e.g. acute opioid overdose, delirium tremens). The specific management of intoxication and withdrawal is specific to the misused substance.
Detoxification and harm minimisation
Detoxification from, and cessation of, the substance is essential if this is an appropriate treatment goal. Once established, supporting relapse prevention for those who achieve abstinence is criticial. This may include both pharmacological and psychological interventions.
Where drug abstinence is not possible, practices are implemented that aim to reduce the harm associated with drug use. This is known as harm minimisation. It aims to reduce the adverse health, social, and economic consequences for the individual, their families, and the wider community. Harm minimisation practices include regular contact with community drug and alcohol services, helping the individual deal with drug-related problems, encouraging health-related behaviours, needle syringe exchange programmes, encouraging the reduction of drug use, and opioid substitution therapy.
Managing co-morbidities
Individuals with substance dependence are likely to have co-morbid physical and mental health issues that may or may not be related to the substance use. These should be screened for, identified, and managed appropriately. Basic lifestyle advice including diet, exercise, and sleep hygiene should be given to all patients.
Risk assessment
Risk assessment involves addressing an individual's risk of harm to self, harm to others, and harm from others. Individuals with substance misuse may be at higher risk of deliberate self-harm, accidental self-harm, and suicide. They may also be more vulnerable to the risk of harm from others and at risk of causing harm to others (including indirect harm to children they are responsible for). The impact of substance use on dependent children needs to be addressed and usually, a safeguarding should be raised to Social Services.
Prognosis
Treatment of alcohol dependence has the highest rate of success.
Of the 110,095 people who left drug and alcohol treatment from 2020-2021, 50% completed their treatment successfully. Those in treatment for alcohol dependence had the highest rate of treatment success at 62%. Those in treatment for opioid dependence had the lowest rate of treatment success at 25%. Substance misuse and dependence is a chronic relapsing-remitting disorder with high relapse rates.
Substance misuse and dependence is associated with high morbidity and mortality. There is a worse prognosis in those with coexisting conditions such as mental health problems or cognitive impairment. The main causes of drug-related deaths are overdose, suicide, violence, accidents, and physical health complications of drug misuse. From 2020-2021 there were 3726 recorded deaths in treatment, representing 1.4% of all people in treatment. People with opioid dependence accounted for 65% of these deaths. Those with alcohol dependence accounted for 29% of these deaths.
Last updated: January 2024
References:
Adult substance misuse treatment statistics 2020 to 2021: report - GOV.UK (www.gov.uk)
Have comments about these notes? Leave us feedback