Benign breast lumps
Notes
Overview
Benign breast lumps are common and can occur in women of all ages.
Lumps in the breast can broadly be divided into benign and malignant. A malignant lump in the breast is known as breast cancer and is discussed in our note on Breast cancer. Benign breast lumps are non-cancerous growths or masses that can develop in the breast tissue. These breast lumps are common and more frequently found in younger women. Diseases of the breast that can result in benign breast lumps include the following:
- Breast cysts
- Fibrocystic changes
- Galactocoele
- Fat necrosis
- Fibroadenoma
- Mastitis and breast abscesses
In this note, we will discuss the broad classification, aetiology, and clinical features of benign breast lumps with a particular focus on cysts, fibrocystic changes, Galactocoele, and fat necrosis. We will then discuss the diagnosis and investigations including key referral criteria before discussing the management of each condition.
Terminology
There are several important medical terms that will help with understanding benign conditions of the breast.
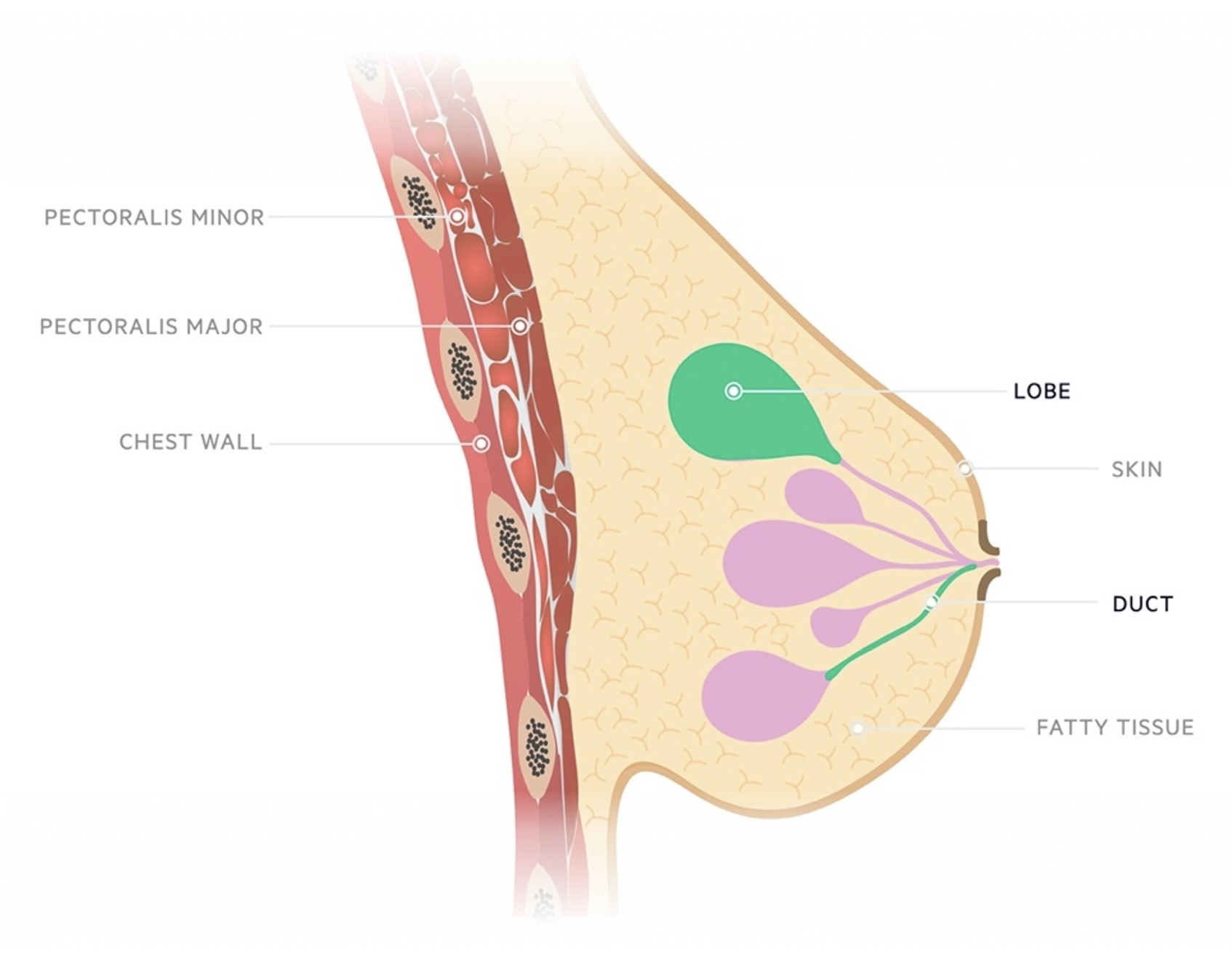
First, benign conditions of the breast may arise from the cells lining the ducts (i.e. ductal) or cells lining the lobes (i.e. lobular).
Second, there may be an increase in cellular growth:
- Proliferative: related to excessive growth (proliferation) of cells.
- Hyperplasia: increase in size of an organ or tissue due to excessive proliferation of cells and an increase in the number of cells. (cf. “hypertrophy” – an increase in the size of an organ or tissue due to an increase in the size of each cell).
Third, cells within the breast may undergo abnormal changes:
- Atypia: the presence of one or more histological features that differ from that of a normal cell of the same type. Sometimes used interchangeably with dysplasia.
- Dysplasia: the presence of one or more histological features that differ from that of a normal cell of the same type. Sometimes used interchangeably with atypia.
- Carcinoma: a cancer that develops from epithelial cells.
- Carcinoma in situ: cells that look like cancer cells under the microscope, but which are only found in the place where they first formed i.e. they haven’t spread to nearby tissue. There is usually a risk of carcinoma in situ progressing to invasive carcinoma.
Epidemiology
Breast lumps are common and may be seen in women of all ages.
Knowledge of breast lumps is important since they are common:
- An estimated 3% of GP visits by female patients relate to a breast mass or breast pain.
- An estimated 50% of women will experience a benign breast lump during their lifetime.
Fortunately, at least 90% of all breast masses are benign.
Classification
Breast masses may be classified as benign or malignant.
We can classify benign breast masses into four main categories, as follows:
- Nonproliferative Breast Masses
- Proliferative Breast Masses Without Atypia
- Proliferative Breast Masses With Atypia
- Miscellaneous Breast Masses
Nonproliferative Breast Masses
- Breast cysts
- Fibrocystic changes
- Galactocoele
Proliferative Breast Masses Without Atypia
Proliferative Breast Masses With Atypia
- Atypical Ductal Hyperplasia
- Atypical Lobular Hyperplasia
- Lobular Carcinoma In Situ
For more information, see our note on Breast cancer.
Miscellaneous Breast Masses
- Fat Necrosis
Aetiology & pathophysiology
Common benign breast lumps include cysts, fibrocystic change, and fibroadenomas.
Another common cause of a benign breast lump is lipoma, which refers to a soft, fatty lump and is typically painless.
Breast Cysts
Breast cysts arise when the drainage from a Terminal Duct Lobular Unit (TDLU) becomes blocked.
The TDLU is the smallest functional unit in the breast, in the same way that the alveolus is the smallest functional unit of the lungs. Each TDLU measures 1-4 mm and comprises:
- Lobules: made up of acini (i.e. secretory epithelial cells) and intralobular terminal ducts which connect the acini within each lobule.
- Extralobular terminal ducts: ducts that connect each lobule with the larger mammary ducts.
Once drainage is blocked, fluid will begin to accumulate in the ducts, forming a round or ovoid mass. In the case of breast cysts, the fluid that accumulates is similar in composition to tissue fluid or plasma (cf. a galactocoele, in which accumulated fluid resembles breast milk).
Fibrocystic Changes
Fibrocystic changes involve two types of changes:
- Fibrosis (i.e. thickening of breast tissue)
- Cyst formation: due to changes in hormone levels during the menstrual cycle.
Since fibrocystic changes are caused by hormone fluctuations, they are most common in menstruating women (especially between the ages of 30-50). Over 50% of women will experience fibrocystic changes.
Galactocoele
Just like breast cysts, galactocoeles occur when drainage of TDLUs become blocked. The main way galactocoeles differ from breast cysts is that they contain breast milk rather than just tissue fluid.
Since galactocoeles can only occur in lactating women, they affect women around times of breastfeeding, including pregnancy, and in the period after weaning.
Common causes of duct blockage in lactating women include mastitis or oedema, both of which can put external pressure on the mammary ducts.
Fat Necrosis
Fat necrosis is the result of interrupted oxygen supply to fat cells in the breast. The two most common causes of such interruption are:
- Breast trauma (e.g. seat belt injury during a road traffic collision)
- Breast surgery: including biopsy, augmentation, reduction, or reconstruction
As a result of the interrupted oxygen supply, fat cells undergo necrosis and saponification, which stimulates a localised inflammatory reaction. The final stage in this inflammatory reaction is the formation of a fibrotic scar.
Clinical features
The history and examination findings alone are usually not sufficient to differentiate between benign and malignant breast lumps.
As a general rule, the history and physical examination alone are not sufficient to differentiate between benign and malignant breast masses. In fact, studies have shown that even experienced clinicians cannot reliably differentiate benign and malignant lesions based on history and examination alone. For this reason, breast masses should always be referred for triple assessment as per NICE guidelines (see Diagnosis and Investigations below).
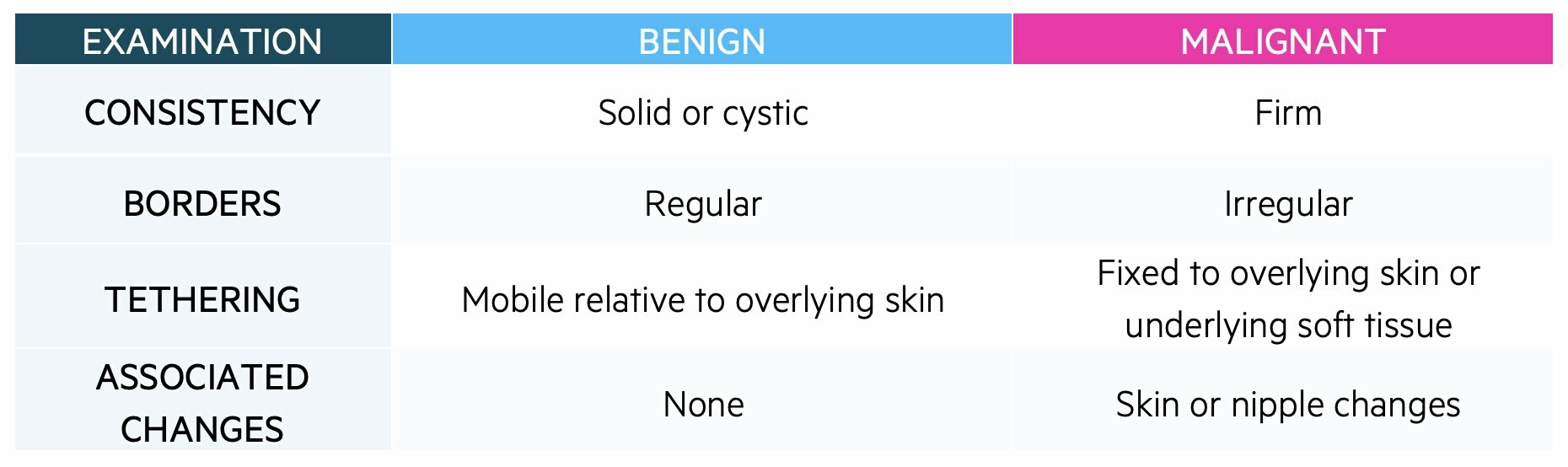
Benign versus malignant
Some features on examination point more generally towards benign or malignant lesions:
History
Other features in the history point towards specific conditions:
- Breast cysts: can be painful or painless. May vary in size across the menstrual cycle.
- Fibrocystic changes: pain usually worst premenstrually, improving after the start of menses.
- Galactocoele: usually during pregnancy, breastfeeding, or shortly after weaning. Typically painless.
- Fat necrosis: trauma (e.g. seatbelt injury or blunt injury), breast biopsy, or surgery
Examination
It is important to determine how firm a lump is and whether it is tethered to underlying structures.
- Breast cysts: usually a single (i.e. simple) cyst, which is smooth, firm, discrete, and often tender
- Fibrocystic changes: diffuse, bilateral nodularity.
- Galactocoele: smooth, well-defined mobile mass. Non-tender.
- Fat necrosis: can mimic malignancy (e.g. irregular edges, non-mobile, tethering).
Diagnosis & Investigations
The majority of patients with breast lumps should be referred for triple assessment.
The vast majority of patients with a breast lump should be referred for triple assessment. This means a complete history, formal examination, and then followed by imaging assessment of the mass/lump with or without sampling to determine histology. The urgency of the referral will depend on the constellation of clinical features and the age of the patient.
Referral pathways
As per NICE guidelines, referrals along suspected cancer* pathways should be actioned as follows:
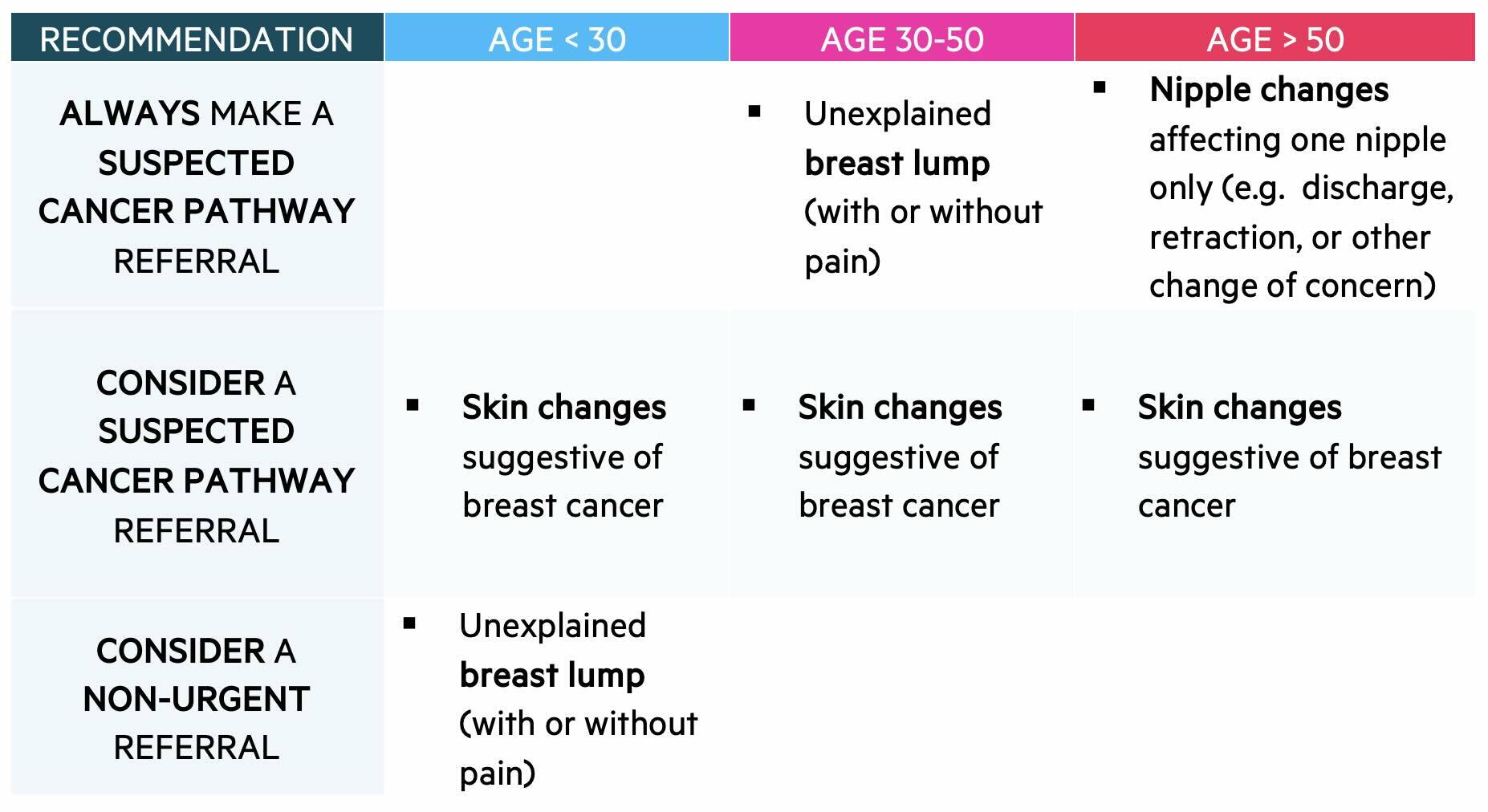
*Suspected cancer pathways used to be known as 2-week wait referrals – you may hear this term used in clinical practice.
Investigations
Patients seen via the suspected cancer pathway will undergo triple assessment. Typical imaging modalities used during triple assessment include ultrasound and mammogram. This is usually followed by sampling of the suspected lesion with biopsy or aspiration unless a clear and confident diagnosis can be made on imaging.
The following investigation results point toward specific benign conditions:
- Breast cyst
- Ultrasound is frequently used to differentiate simple cysts (i.e. a single, homogenous fluid-filled compartment) from complicated cysts (i.e. containing debris) and complex cysts (i.e. containing septations or solid components).
- Biopsy may or may not be performed based on the ultrasound findings:
- Simple cysts are usually benign lesions, and do not need to be biopsied. Fine needle aspiration (FNA) may be performed to exclude infection if there are signs of the cyst being infected.
- Complicated cysts are usually benign lesions, and do not need to be biopsied. Occasionally complicated cysts might appear higher risk for malignancy – in this case, they may undergo FNA.
- Complex cysts might represent malignancy, and so they are usually biopsied using core needle biopsy (CNB). CNB is preferred over FNA in this situation, since CNB will obtain samples of septations and solid components within the cyst, which FNA could miss.
- Fibrocystic changes
- A diagnosis of exclusion – mammography, ultrasound and/or biopsy may be performed to exclude other more sinister conditions.
- Galactocoele
- Aspiration is often performed. The aspirate will reveal milk if the cyst formed recently. If the cyst is older, the aspirate may appear thickened.
- Fat necrosis
- Fine needle biopsy or core needle biopsy will reveal features of necrosis and associated inflammatory changes, such as ‘foamy macrophages’ and lymphocytes.
Management
Management of benign breast lumps depends on the underlying condition.
Breast cysts
The treatment of breast cysts will depend on whether they are simple, complicated, or complex.
- Simple Cysts: Usually require no specific treatment. If especially large and uncomfortable, therapeutic fine needle aspiration can be performed. A drained simple cyst does not usually refill.
- Complicated Cysts: Usually require no specific treatment.
- Complex Cysts: Once malignancy has been excluded, patients should be followed up every 6-12 months for 1-2 years to ensure the cyst is stable (i.e. not growing or changing rapidly).
Fibrocystic changes
The management of breasts with fibrocystic change can be divided into conservative, medical, and surgical.
- Conservative
- Apply warm or cool compresses to breasts.
- Wear a comfortable, supportive bra.
- Avoid large amounts of salt, fat, or caffeine in the diet, which may worsen symptoms.
- Medical
- Simple analgesia – paracetamol or ibuprofen.
- Oral contraceptives – these lower the levels of cycle-related hormones, and so can reduce fibrocystic breast changes.
- Surgical
- Therapeutic fine needle aspiration of larger, painful cysts.
- Persistent cysts that do not resolve after repeated aspirations may be surgically excised.
Galactocoele
Usually not required as the majority resolve spontaneously.
Fat necrosis
Usually not required.
If fat necrosis is causing pain or distortion of the shape of the breast, surgical removal can be performed.
Prognosis
Non-proliferative breast masses are not associated with an increased cancer risk.
In general, non-proliferative breast masses non-proliferative breast masses such as breast cysts, fibrocystic changes, or galactocoeles are not associated with an increased risk of cancer. The risk of subsequent breast cancer in patients with high-risk complicated cysts and complex cysts depends upon biopsy results. Fat necrosis, which is a miscellaneous breast mass, is not associated with an increased cancer risk.
Last updated: August 2024
References:
UpToDate: Clinical manifestations, differential diagnosis, and clinical evaluation of a palpable breast mass.
UpToDate: Breast cysts: Clinical manifestations, diagnosis, and management.
UpToDate: Overview of benign breast diseases.
NICE guideline: [NG12] Suspected cancer: recognition and referral
Eberl, MM, et al. Characterizing breast symptoms in family practice. Ann Fam Med. 2008 Nov-Dec;6(6):528-33. doi: 10.1370/afm.905. Accessed 08/05/2024
Walker S, et al. Risk of breast cancer in symptomatic women in primary care: a case-control study using electronic records. Br J Gen Pract. 2014 Dec;64(629):e788-93. doi: 10.3399/bjgp14X682873. Accessed 08/05/2024
Sanfrancesco J, et al. Diagnostically challenging cases: what are atypia and dysplasia? Urol Clin North Am. 2013 May;40(2):281-93. doi: 10.1016/j.ucl.2013.01.006. Accessed 08/05/2024
Radiopedia. Liao, A. Fat necrosis (breast). Accessed 10/05/2024
Have comments about these notes? Leave us feedback
