Acute otitis media
Notes
Overview
Acute otitis media (AOM) refers to inflammation of the middle ear with effusion and clinical features of a middle ear infection.
Normally AOM is a self-limiting condition, commonly occurring in children, though adults can also be affected. In general symptoms settle after 3 days, but can remain for a week. Bacteria or viruses are normally implicated - differentiating the two is challenging.
The majority of cases do not require antibiotic therapy and will settle with time. Though rare, serious complications such as mastoiditis, meningitis, intracranial abscess, sinus thrombosis or facial nerve paralysis may occur.
AOM may become persistent or recurrent. NICE defines persistent and recurrent AOM as follows:
- Persistent AOM: patients with a single episode of AOM who re-present with persistent or worsening symptoms.
- Recurrent AOM: three or more distinct episodes of AOM in the past six months, or four or more in the past twelve months, one of which was in the last six months.
Epidemiology
AOM occurs primarily in children but may also affect adults.
Children aged 0 to 4 years are most affected, with a peak in the incidence at around 9-15 months. It is more commonly seen in winter and is often associated with an upper respiratory tract infection.
Aetiology
AOM is commonly caused by viruses, bacteria or both.
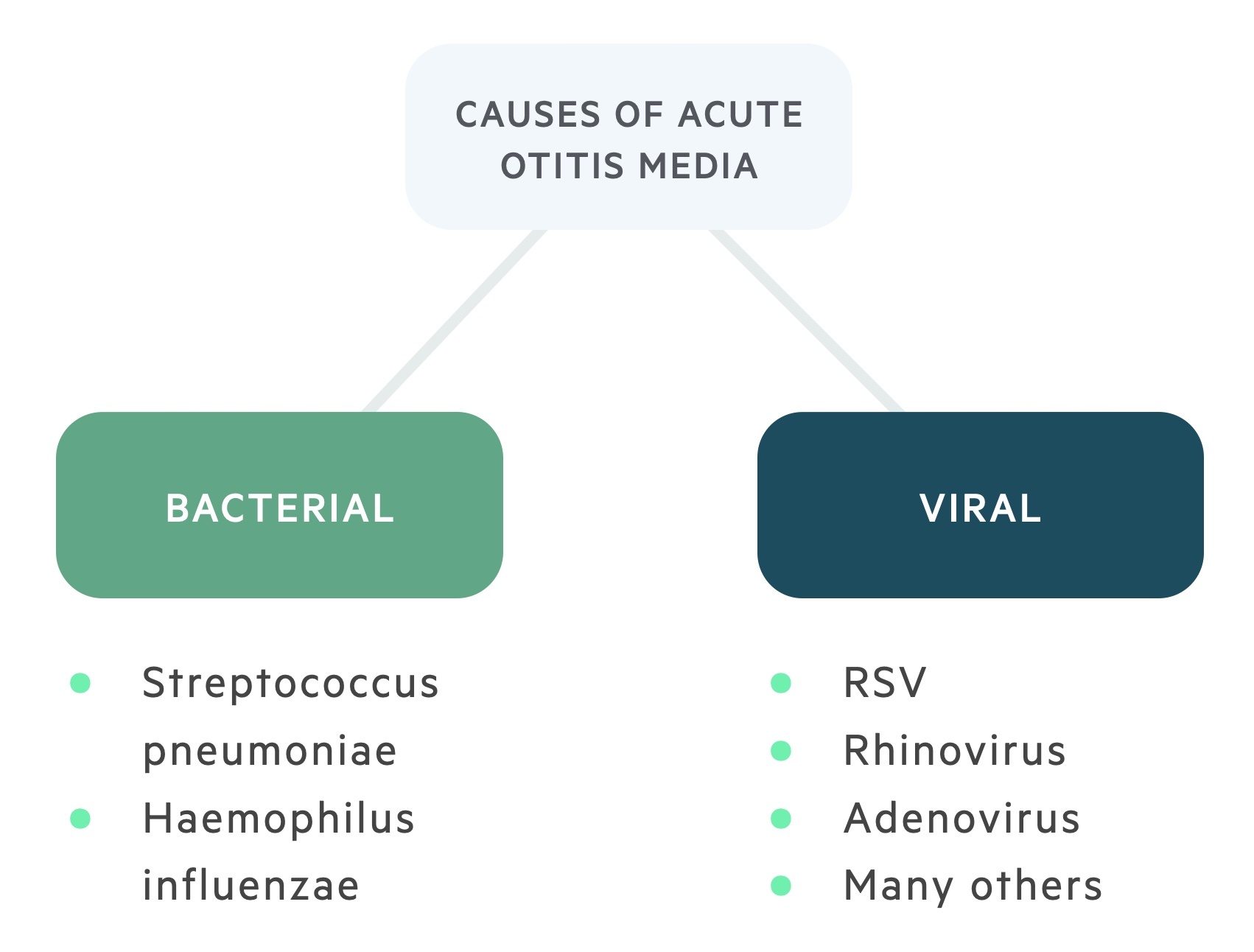
Commonly identified bacteria include:
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis
- Streptococcus pyogenes
Streptococcus pneumoniae is thought to be the most common bacterial cause followed by Haemophilus influenzae.
Commonly identified viruses include:
- Respiratory syncytial virus
- Rhinovirus
- Adenovirus
- Influenza virus
- Parainfluenza virus
Pathophysiology
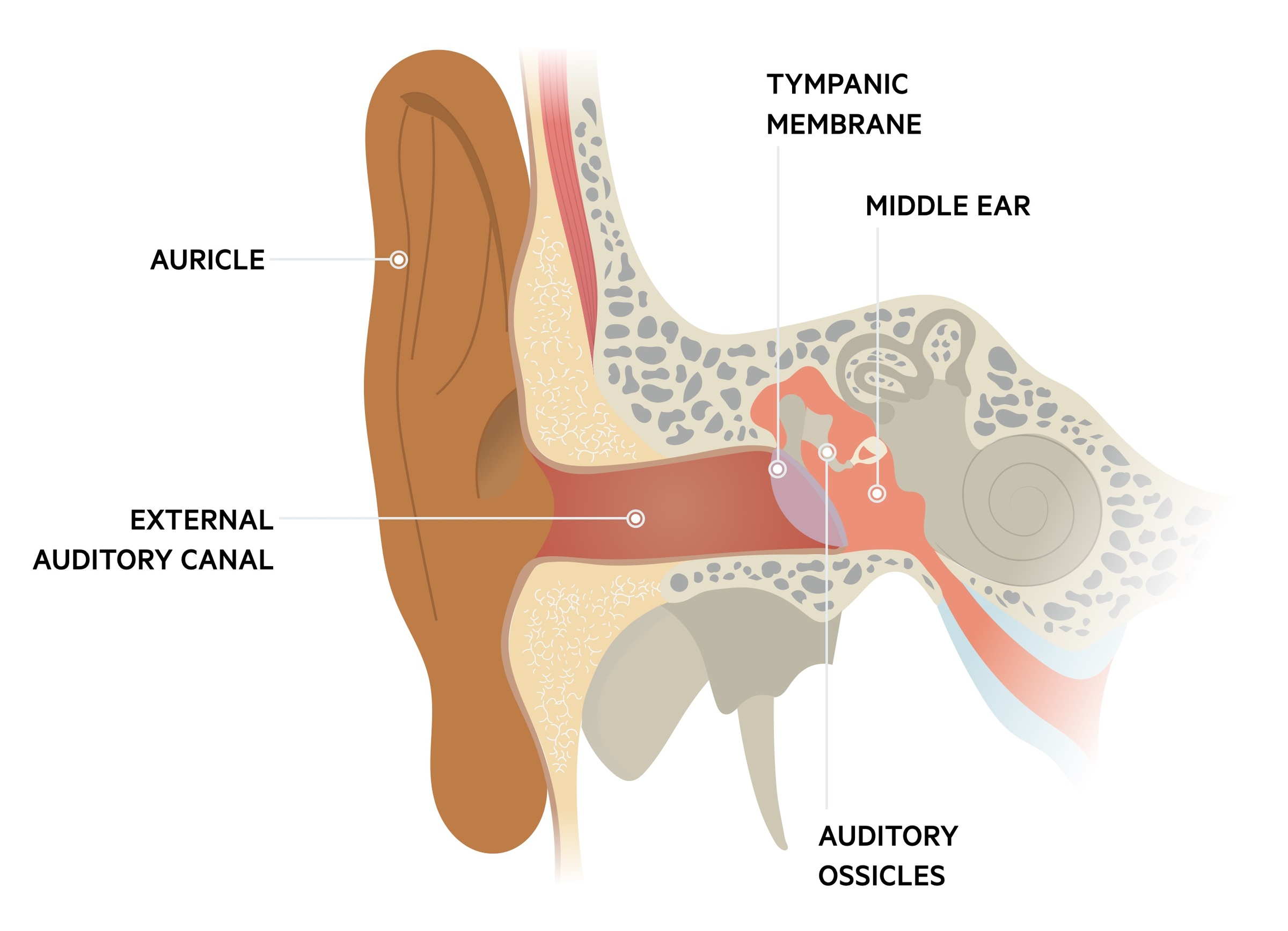
Infective organisms reach the middle ear via the eustachian tube.
AOM is often associated with a preceding upper respiratory tract infection. Pathogen transmission via the eustachian tube to the middle ear may result in AOM.
It is thought that in young children the less acute angle of the eustachian tube within the wall of the pharynx results in increased transmission of pathogens, particularly when coughing or sneezing.
Clinical features
Otoscopy is key to diagnosing AOM.
Signs and symptoms depend somewhat on the age group of the presenting patient. Remember features of an upper respiratory tract infection may be present.
Symptoms
Neonates
- Irritability
- Difficulty feeding
- Fever
Young children
- Holding or tugging ear
- Irritability
- Fever
Older children and adults
- Otalgia (ear pain)
- Hearing loss
- Fever
Otoscopy
Otoscopy is key to identifying signs of AOM. It allows for visualisation of the tympanic membrane, behind which the middle ear lies. The normal tympanic membrane has a slight translucency with a colour sometimes described as pearly-grey. The malleus (the first of the three bones of the middle ear) is clearly visible.
In AOM a number of changes may be seen:
- Red, yellow or cloudy tympanic membrane
- Bulging tympanic membrane or perforated membrane
- Air-fluid level behind the tympanic membrane
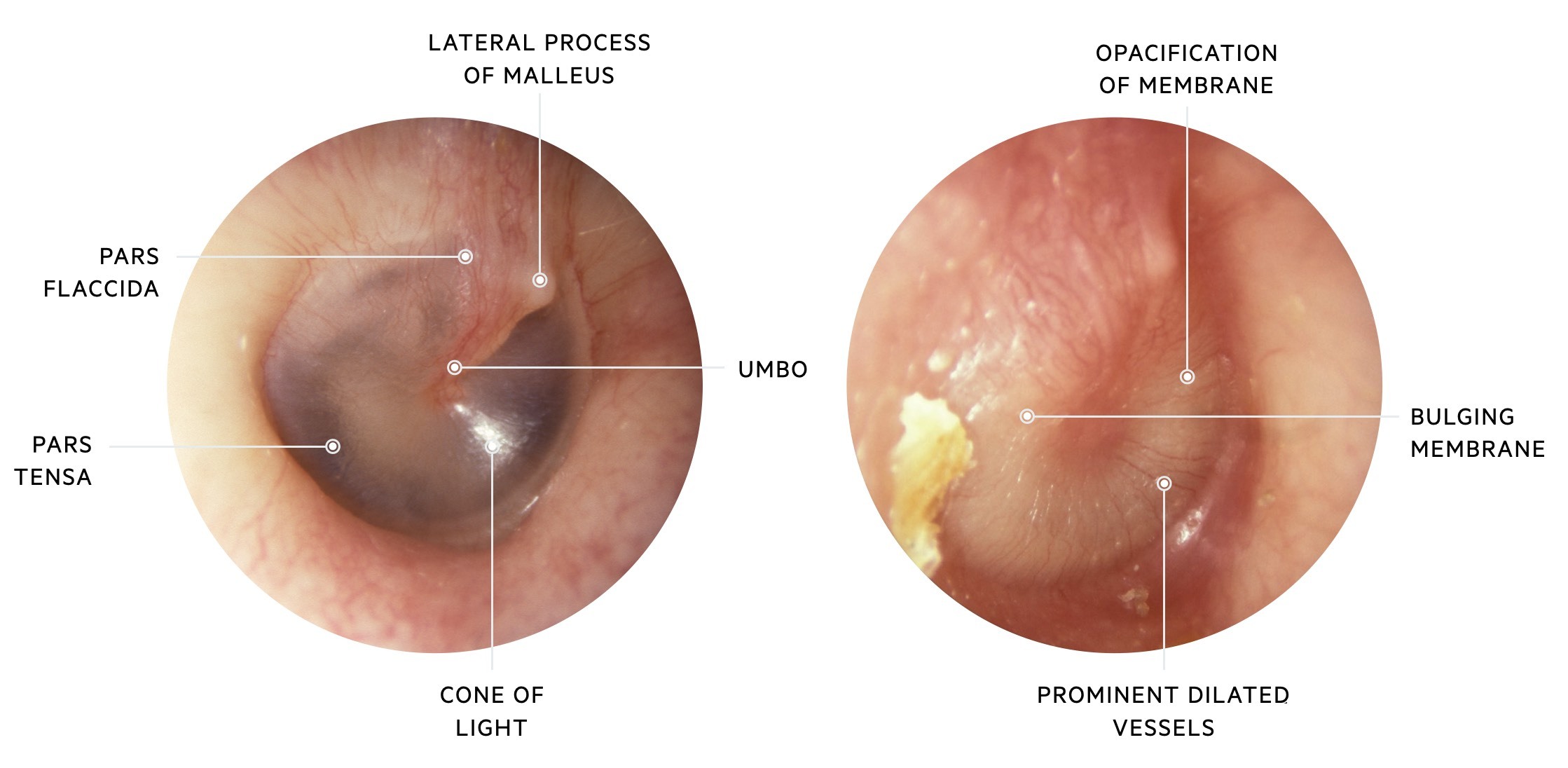
Left: a view of a normal right tympanic membrane. Right: a view of a right tympanic membrane with changes consistent with otitis media
Images courtesy of Michael Hawke MD and CC 4.0
Management
AOM has a spectrum of severity from a self-limiting illness to severe systemic upset requiring hospital admission.
General advice
Explain the condition to the patient and their family, as well as the fact that it is generally self-limiting. Normally the illness lasts 3 days but it may last up to a week.
Analgesia and antipyretics are advised. Paracetamol and ibuprofen (in absence of contra-indications) at appropriate doses can be used.
Antibiotics
As described above, most cases of AOM are self-limiting. Overuse of antibiotics risks both adverse effects for the patient and increasing antibiotic resistance. There are three main approaches for antibiotic prescribing in AOM:
- No antibiotics
- Delayed prescription
- Immediate antibiotics
In all cases give safety netting advice to return if symptoms worsen, do not improve after 3 days or the patient becomes systemically unwell.
When giving a delayed or backup prescription advise using if symptoms don’t improve after 3 days or if they worsen (rapidly or significantly).
Where antibiotics are indicated, amoxicillin tends to be preferred first-line (in absence of penicillin allergies) as a 5-7 day course, with alternatives including clarithromycin and erythromycin. Co-amoxiclav (combination of amoxicillin and clavulanic acid) is used second line (again in the absence of penicillin allergies) in treatment-resistant cases.
NICE guidelines NG91: Otitis media (acute): antimicrobial prescribing, offers guidance to GPs on which children and young people may require antibiotics:
- In ‘Children and young people who are systemically very unwell, have symptoms and signs of a more serious illness or condition, or are at high-risk of complications.’ immediate antibiotic therapy is advised. The need for urgent hospital admission should be considered (see below).
- In ‘Children and young people who may be more likely to benefit from antibiotics (those of any age with otorrhoea or those under 2 years with infection in both ears).’ consider either no antibiotics, a backup script for antibiotics or immediate antibiotics.
- In ‘Children and young people who may be less likely to benefit from antibiotics.’ consider either no antibiotics or a backup script.
Who to admit?
As always clinical judgement should be used when making decisions on the best place of care. Clinicians must consider the severity of the presentation (and any complications that may be present), home dynamics and any co-morbidities. The majority of patients will be safely treated in the community.
NICE guidelines recommend that children and young people should be admitted in the following situations:
- Evidence of a severe systemic infection
- Evidence of an acute complication: mastoiditis, meningitis, intracranial abscess, sinus thrombosis or facial nerve paralysis.
Persistent AOM
Patients with persisting (or worsening) symptoms should be reviewed. Repeat a complete history and re-examine. Consider other potential causes of similar symptoms such as otitis media with effusion (‘glue ear’). In general, management follows the outline described above.
Some patients may develop chronic suppurative otitis media (CSOM) as a complication of their AOM. Those with persistent symptoms of AOM should be referred to ENT, particularly if lasting longer than 6 weeks or there is persistent hearing loss.
Recurrent AOM
ENT referral for specialist management should be considered for those with recurrent AOM. This is especially important if there is a craniofacial abnormality, an adult patient, or debilitating/complicated AOM.
If nasopharyngeal cancer is suspected an urgent referral to ENT is required. Some red flag features that may make you concerned for an underlying cause of recurrent AOM include conductive hearing loss between episodes, cervical lymphadenopathy, nasal obstruction or epistaxis.
Complications
Though most cases of AOM resolve without sequelae, some may develop complications.
Frequent complications include:
- Persistent AOM
- Recurrent AOM
- Perforation of tympanic membrane
- Hearing loss
Rarely very serious complications like mastoiditis, meningitis, intracranial abscess, sinus thrombosis and facial nerve paralysis may occur.
Mastoiditis is perhaps the most commonly occurring serious complication. It is a potentially life-threatening infection of the mastoid air cells causing pain, swelling and erythema behind the ear and systemic upset. It tends to affect younger patients, normally under the age of 5. Blood tests, fluid cultures and CT scanning form the core of the work-up. It requires prompt recognition, early antibiotics and management that may include myringotomy (drain the middle ear with a hole in the tympanic membrane) and mastoidectomy (removal of infected tissue/bone).
Last updated: October 2024
Further reading
- NICE guideline 191: Otitis media (acute): antimicrobial prescribing
Have comments about these notes? Leave us feedback