Diverticulitis
Notes
Overview
Diverticulitis is characterised by acute inflammation and infection of diverticula.
Diverticulitis is a common presentation on any surgical take. It typically presents with abdominal pain and fevers.
Terminology is key to understanding diverticulitis and its associated diseases:
- Diverticula: Sac like protrusion of the colonic mucosa through the muscular wall.
- Diverticulosis: The presence of asymptomatic diverticula.
- Diverticular disease: Symptomatic diverticula (e.g. abdominal pain) in the absence of inflammation. Also used as an umbrella term.
- Diverticulitis: Symptomatic acute inflammation and infection of diverticula.
Diverticulosis most commonly affects the sigmoid colon but may occur anywhere in the gastrointestinal tract. Right sided colonic disease is more common in those of Asian descent.
Epidemiology
Diverticulosis affects around 80% of those aged 85 or older.
The incidence of diverticulosis increases with advancing age. It is rare before 40, above the age of 45 it affects 5-10% and above the age of 85 it will affect up to 80%.
The majority of individuals with diverticulosis will remain asymptomatic. However for patients with diverticulosis the lifetime risk of acute diverticulitis is 4-25%.
Risk factors
A number of risk factors are associated with diverticulosis and acute diverticulitis.
- Diet: Diets high in red meat and low in fibre appear to be associated with diverticular disease and diverticulitis
- Obesity
- Family history
- Smoking: Increased risk of diverticulitis and diverticular bleed
- Medications: NSAIDs, steroids have been associated with increased risk of diverticular perforation
Pathophysiology
Diverticula are thought to occur due to raised intra-luminal pressures and abnormal colonic motility.
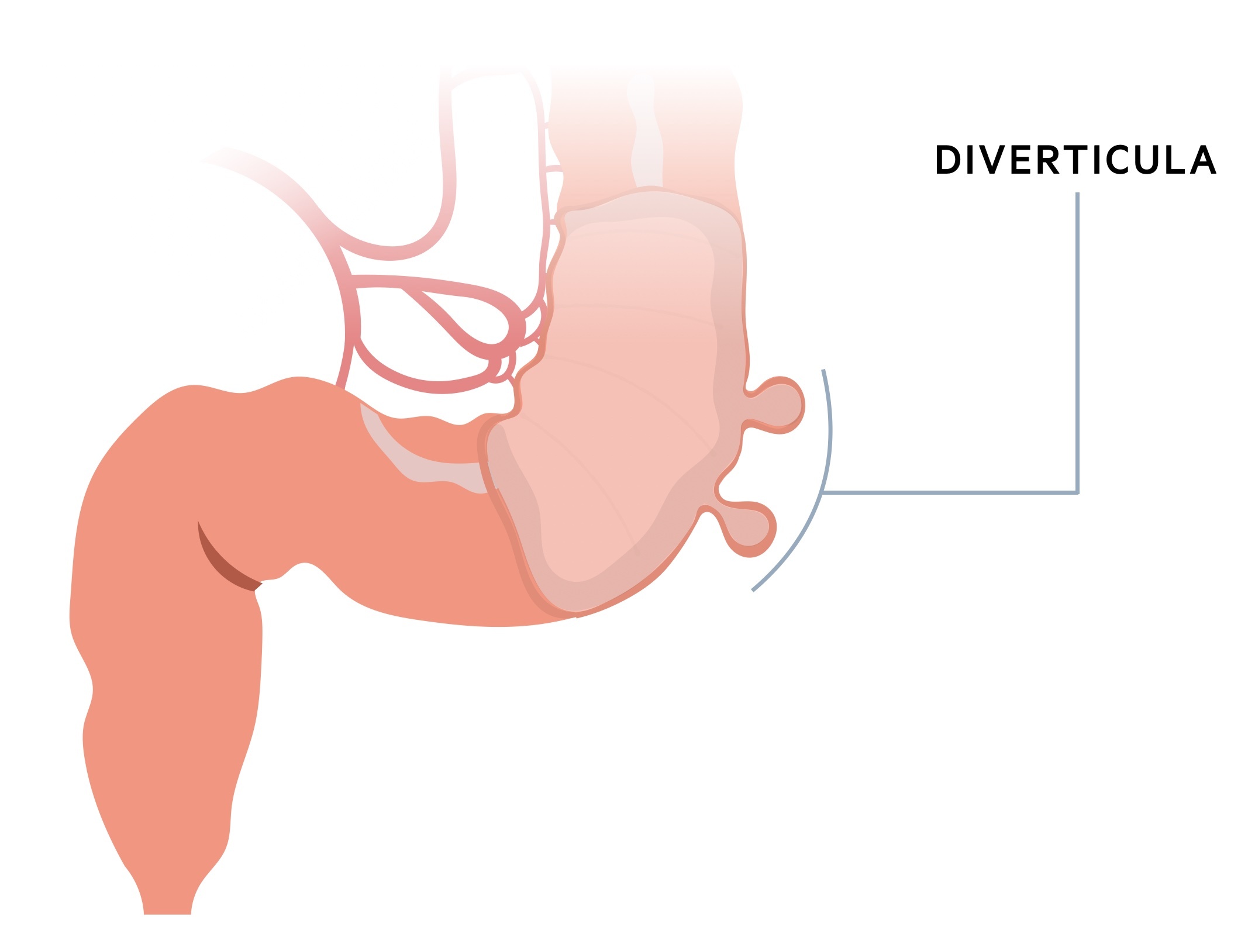
Diverticula
Diverticula occur when the colonic mucosa (and submucosa) protrudes through the muscular layer (muscularis externa) so to only be covered by the serosa. They appear to occur in weak areas, at points where vasa recta penetrate the muscularis externa.
Diverticula become increasingly common with advancing age. Though it is not known exactly why they occur, it is thought to be related to raised intra-luminal pressures and abnormal colonic motility.
Diverticulitis
Not everyone with diverticula develop diverticulitis, it is estimated that patients with diverticulosis have a 4-25% lifetime risk of acute diverticulitis. The exact cause of diverticulitis is still unknown although a number of theories have been posited.
It is thought to occur due to perforation of diverticula, this may be microscopic (and without signs like free air in the abdomen) or macroscopic. The perforation is said to occur due to food particles or raised intra-luminal pressures.
There is a wide-range of clinical presentations. Microscopic perforations may result in mild localised inflammation which is quickly walled off by mesentery/omentum. In more severe cases generalised purulent or faecal peritonitis occurs.
Further complications can occur. Prolonged inflammation between the colon and a neighbouring organ (e.g. bladder) may result in a fistula. Recurrent episodes of diverticulitis may result in diverticular strictures and obstruction.
Clinical features
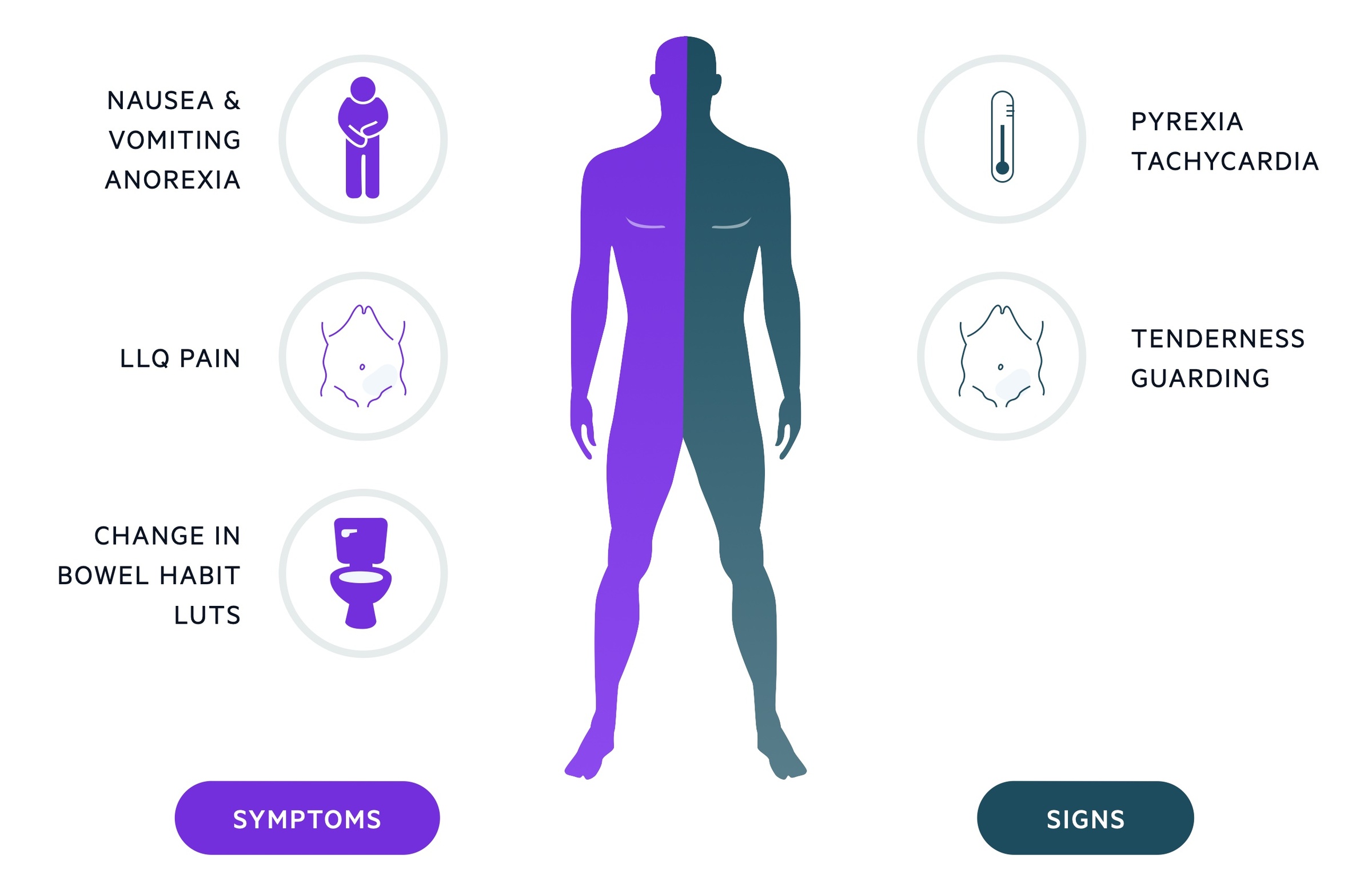
Patients often present with abdominal pain, fevers and tenderness in the left iliac fossa.
Symptoms
- Abdominal pain
- Pyrexia
- Change in bowel habit
- Nausea
- Anorexia
- Urinary frequency
Signs
- Abdominal tenderness
- Guarding / peritonism
- Palpable mass (uncommon)
- Tachycardia
- Haemodynamic instability (uncommon)
Investigations & diagnosis
CT abdomen and pelvis is the imaging modality of choice to diagnose diverticulitis.
Bedside
- Observations
- Urine dip
- Pregnancy test
Bloods
- FBC
- U&Es
- LFTs
- Amylase
- CRP
- Group & save
- Clotting screen
Imaging
CT Abdomen and pelvis: The diagnostic modality of choice. Helps to assess severity (along with clinical signs), prognosis and identify complications. Should be with contrast unless contraindicated.
Modified Hinchey classification
The modified Hinchey classification can be used to help guide the need for surgical intervention.
I A: Confined pericolic inflammation/phlegmon
I B: Confined pericolic abscess
II: Pelvic, retroperitoneal or distant intraabdominal abscess
III: Generalised purulent peritonitis
IV: Generalised faecal peritonitis
Management
Diverticulitis presents with a spectrum of severity which dictates management.
Outpatient management
- Who?: Consider management in the community if the patient is young, healthy and well, with mild, uncomplicated disease and controlled pain.
- Antibiotics: A 7-10 day course of antibiotics should be prescribed, typically co-amoxiclav (in the absence of penicillin allergy). Alternatives include ciprofloxacin and metronidazole.
- Analgesia: Paracetamol is recommended for analgesia. Try to avoid NSAIDs and opioids. Increased risk of complications.
- Follow-up: Patients managed in the community should be reassessed at 48 hours and given appropriate safety-net advice. Outpatient colorectal follow-up and colonoscopy (if appropriate) should be arranged.
Inpatient management
Admit any patient who is elderly, co-morbid, unwell, in significant pain, peritonitic or has evidence of perforation or abscess formation on CT. If features of severe systemic infection are present, urgently arrange senior review, complete the sepsis six bundle and promptly refer to surgeons.
Commence IV antibiotics, co-amoxiclav is normally first line (in the absence of penicillin allergy). The patient should be nil by mouth until surgical review and commenced on intravenous fluids.
Surgical management may be required in those presenting with severe complicated disease or who fail to respond to conservative management. Interventions include radiologically guided drainage of abscess or laparoscopic washout. In more severe cases a Hartmann’s procedure may be required.
Further management
There is a risk of underlying malignancy and as such outpatient colorectal follow-up and colonoscopy (if appropriate, and after acute inflammation has settled) should be arranged at discharge. Those who have undergone resection should receive colorectal follow-up.
Most advise a high-fibre diet (and to avoid constipation) though the evidence that this reduces attacks is not clear.
Elective surgical intervention for those with repeated attacks should be discussed with a colorectal consultant.
Complications
Acute diverticulitis and diverticula are associated with a number of complications.
- Fistula (e.g. colovaginal, colovesical): Repeated or persistent inflammation between two intraabdominal organs may lead to the formation of a fistula - an abnormal connection between two epithelial surfaces.
- Colonic stricture: Repeated episodes of diverticulitis and inflammation leads to scar tissue and stricture formation. They may result in change in bowel habit and large bowel obstruction. See our Bowel obstruction notes for more.
- Diverticular bleed: This normally occurs in the absence of diverticulitis. Diverticula lead to weakening of adjacent vessel walls and resulting bleeding. See our Acute lower GI bleed notes for more.
Last updated: October 2021
Have comments about these notes? Leave us feedback
