Testicular torsion
Notes
Overview
Testicular torsion is a urological emergency, that without intervention leads to ischaemia and loss of the testis.
Testicular torsion is a rare but serious condition. Successful treatment requires prompt recognition, referral and surgical intervention.
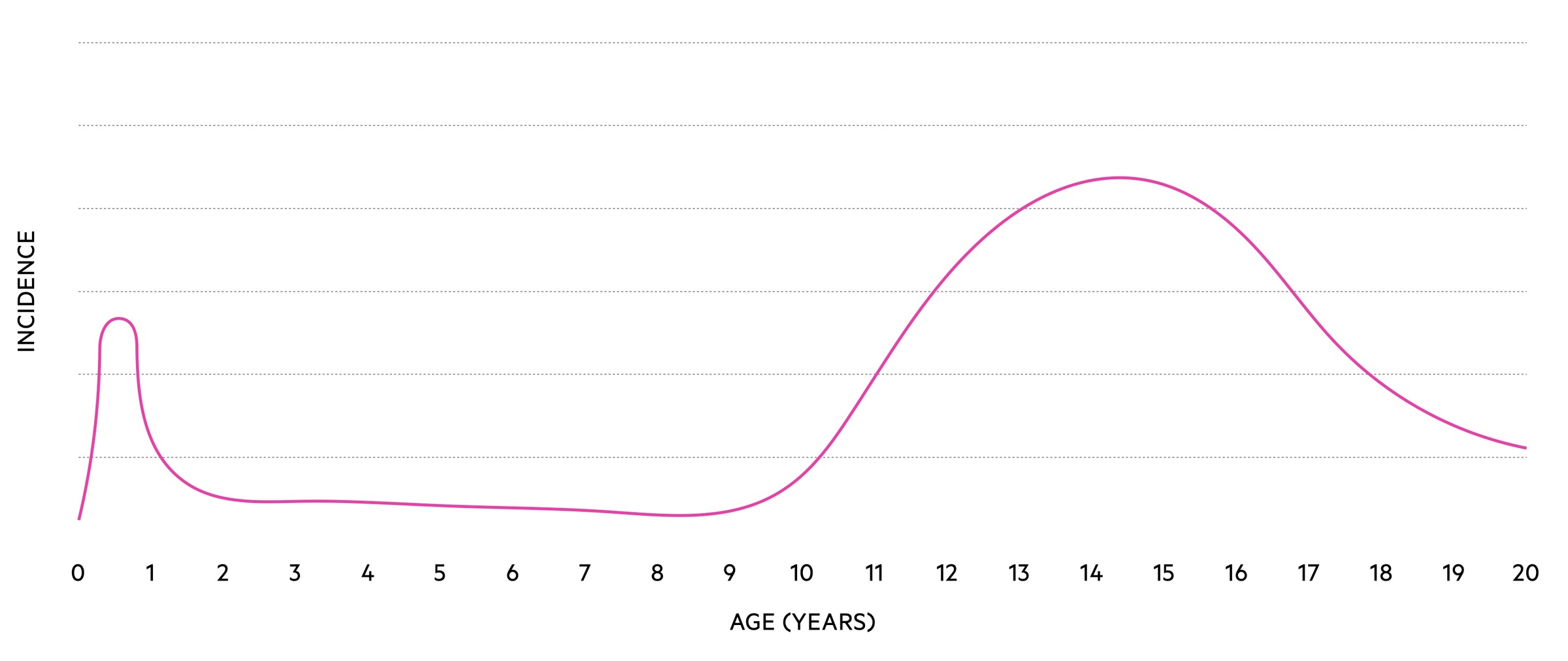
It exhibits a bimodal distribution with peaks in the neonatal period and around puberty.
Differential Diagnosis
Whilst other diagnoses should be considered, suspicion of testicular torsion requires urgent testicular exploration
- Trauma
- Epididymo-orchitis
- Torsion of the epididymal appendage
- Testicular tumour (an association between testicular cancer and torsion has been described)
- Hydrocele
- Inguinal hernia
- Systemic diseases (e.g. Henoch-Schönlein purpura, Mumps)
Types
Testicular torsion may be intravaginal or extravaginal.
Extravaginal torsion occurs in-utero and in neonates. It occurs as the tunica vaginalis is not fixed to the gubernaculum and can tort en masse with the spermatic cord.
Intravaginal torsion occurs due to torsion of the spermatic cord within the tunica vaginalis, it most commonly occurs in adolescence. Patients with a ‘bell clapper’ deformity, where they have a high insertion of the tunica vaginalis, are predisposed to testicular torsion.
Clinical features
Patients will complain of testicular pain, usually with a quick onset.
Pain and swelling are typical features. Of course in young patients and neonates the history may well simply indicate increased distress and clinical findings may raise suspicion of testicular torsion.
The history may also suggest previous similar episodes, this can be indicative of intermittent torsion - detorsion.
Symptoms
- Acute, severe, testicular pain
- Nausea and vomiting
Signs
- Testicular swelling
- Testicular erythema
- Tenderness
- High riding testicle
- Prehn's sign: states that elevation of the affected testicle relives the pain of epididymitis but not of testicular torsion.
- Cremasteric reflex: a reflex caused by stroking the inner thigh leading to cremasteric contraction and elevation of the scrotum on the same size. May be absent in torsion.
The above signs are indicative but cannot conclusively rule in or rule out torsion.
Investigations
Investigations should not delay referral and testicular exploration in cases of suspected testicular torsion.
Bedside
- Vital signs
- Urine dipstick (send MSU)
- Consider sexual health screen (if epididymo-orchitis considered)
- BM (if diabetic or suspected diabetic)
Bloods
- FBC
- UEs
- CRP
NOTE: Unless specifically indicated clotting screens and group & saves are not required.
Imaging
Imaging is not typically indicated or recommended, it can lead to unnecessary delays and the sequelae of a false-negative are significant.
Literature has indicated a reasonable sensitivity and specificity of Doppler USS, though with a great deal of inter-operator variability.
The decision to obtain a USS in equivocal cases should be made by a urology consultant.
Management
Prompt surgical exploration is key, viability of the testicle reduces significantly after 4-6 hours.
Referral
Once suspicion of torsion has been raised, an urgent referral to paediatric surgery or urology should be made. The patient should be made nil by mouth, and appropriate basic investigations obtained.
Surgery
Emergency testicular exploration is indicated in patients with suspected testicular torsion. If confirmed (and the testicle is viable) torsion is managed with detorsion and orchidopexy (fixation of the testicle with sutures). The contralateral testicle should also be explored and fixed in place due to the increased risk of further testicular torsion.
Care should be taken to clearly explain that this is in part a diagnostic procedure and no evidence of torsion (or indeed any pathology) may be found. Additionally, you must explain that orchidectomy may be required if a non-viable testicle is found. An implant can be placed at a later date.
In the setting of a very delayed presentation with a missed testicular torsion, consult with the urology consultant on-call about how to proceed.
Follow-up
Patients, particularly paediatric patients, should be followed up at 6 months for review and assessment of the testis.
In cases of orchidectomy a prosthesis should be offered (though delayed until after puberty if pre-pubescent). Psychological support, for both the patient and their guardian, should be offered.
Complications
Misdiagnosis or incorrect management may result in a number of complications.
Orchidectomy
Required if a non-viable testicle is found on exploration. Viability drops off rapidly after 6 hours from the onset of symptoms. If < 6 hours viability is approximately 90%, this falls to around 10% at 24 hours. The degree of torsion impacts this, a 360-degree twist may result in testicular necrosis in under 4 hours.
Delayed testicular atrophy
May occur even after successful detorsion with a viable appearing testicle. Again risk is increased the greater the delay to surgery.
Recurrence
Unfortunately, orchidopexy does not guarantee torsion cannot recur though rates are estimated to be < 5%. There remains debate and differing practice in exact fixation techniques and suture material used.
Fertility
Some studies have shown impaired semen in patients undergoing delayed surgery. Most men will not have trouble conceiving following an orchidectomy providing the remaining testicle is healthy.
Last updated: November 2021
Have comments about these notes? Leave us feedback
